
Getty Images
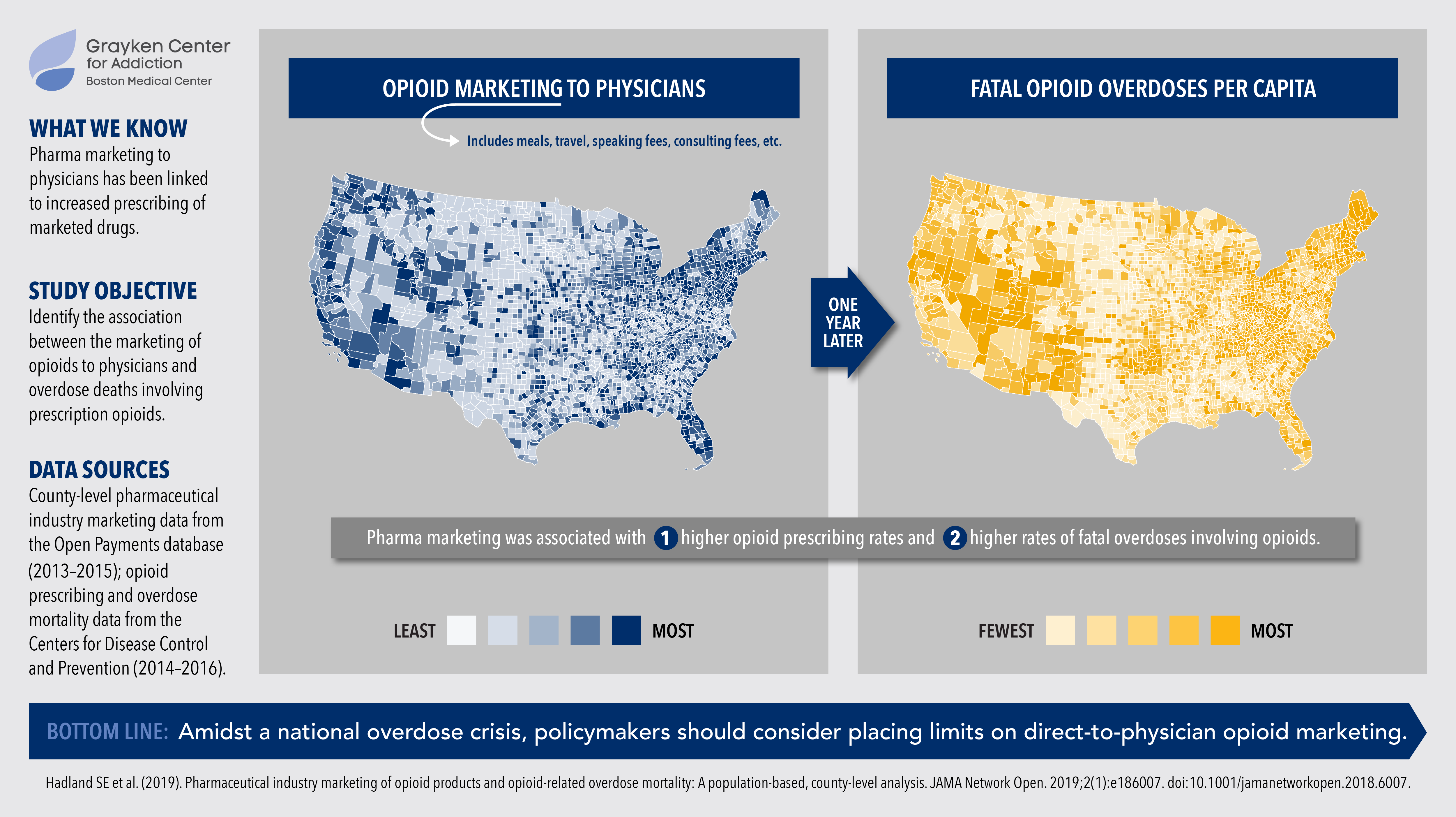
A new county-by-county analysis finds that opioid marketing is associated with higher prescribing rates and higher rates of fatal overdoses one year later.
The link between direct-to-physician pharma marketing and increased drug prescribing has been well documented in research and media reports. The marketing-prescribing connection for opioid drugs in particular has been far less clear, however — an important blind spot in our understanding of the ongoing opioid epidemic.
That blind spot just got a lot smaller. A new county-by-county analysis from the Grayken Center for Addiction at Boston Medical Center has found that opioid marketing is linked to higher opioid prescribing rates nationwide, as well as higher rates of fatal opioid-related overdoses one year later.
A previous study from the same group had linked marketing dollars to an uptick in opioid prescriptions. But this was the first study to find a connection between opioid marketing and opioid overdose deaths.
FAST FACTS
|
Led by pediatrician Scott Hadland, MD, the researchers looked at three different measures of marketing: total dollars spent, number of payments, and the number of physicians involved. Interestingly, the number of payments — including high-touch, low-cost interactions, such as taking physicians out to lunch — was correlated most strongly with fatal overdoses a year later.
The more direct-to-physician marketing a region received, the more overdose deaths it saw, regardless of the total payments, number of doctors, or amount spent.
The findings, published this week in JAMA Network Open, suggest that state regulations that cap high-dollar marketing (such as New Jersey’s limit on annual direct-to-physician marketing expenses to $10,000) would do little to blunt the impact of low-cost, high-volume interactions. Instead, the industry should consider policies that limit volume, not just value, of marketing activities.
“Given the widespread nature of direct-to-physician marketing by opioid pharmaceutical companies, including paying for meals, we must take a hard look at these practices and provide guidance on how they can be better regulated to save lives,” Hadland said.


