Going Inside the Lab That’s Using Zebrafish to Help Blood Cancer Patients
May 1, 2025
By Gina Mantica

Boston Medical Center
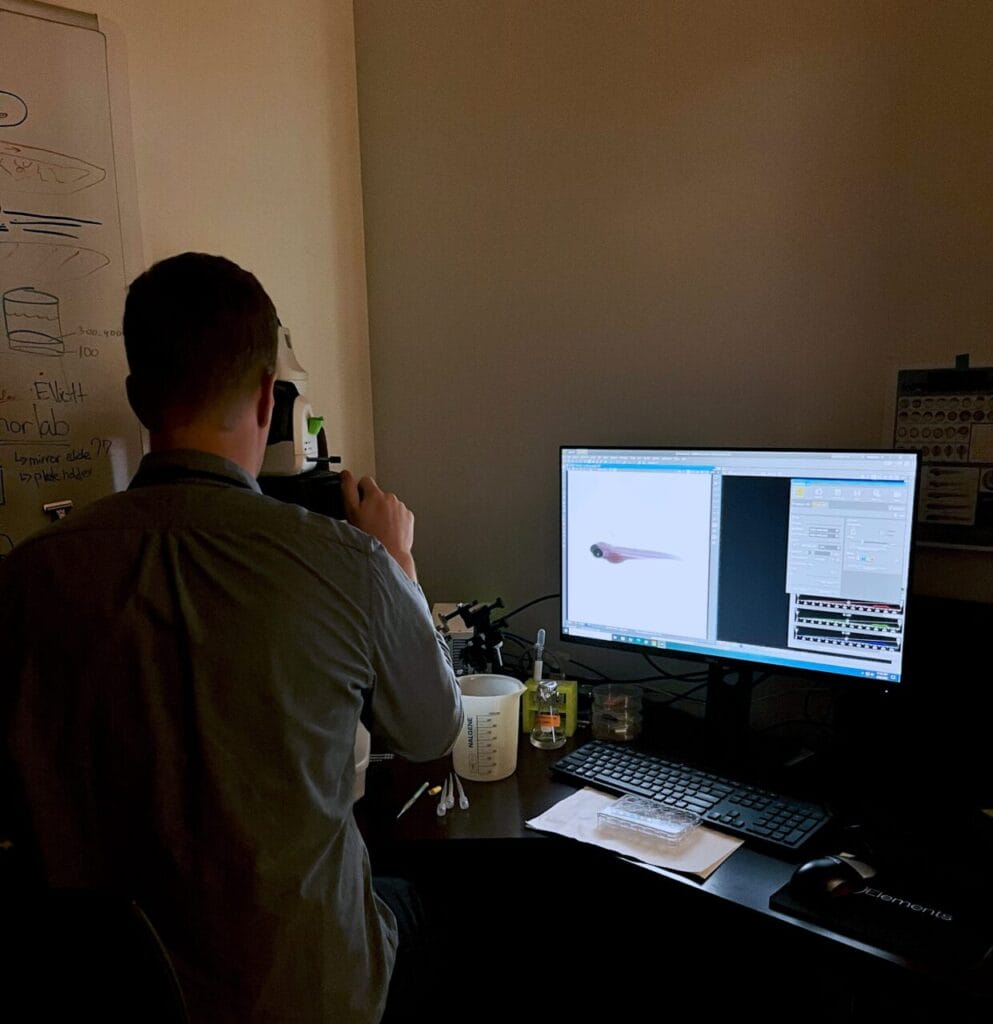
Elliott Hagedorn, PhD, displays zebrafish.
Elliott Hagedorn, PhD, a researcher in Hematology & Medical Oncology and Associate Member of the Center for Regenerative Medicine (CReM), uses zebrafish to uncover how blood stem cells migrate and take root in the body.
Each year, around 18,000 patients are diagnosed with blood cancers or other life-threatening conditions where a bone marrow or hematopoietic stem cell transplant is their best treatment option. While these transplants can save lives, they come with significant risks: In the weeks and months after the procedure, patients are left severely immunocompromised with weakened defenses against infection.
To improve recovery after transplant, scientists are turning to developmental biology for answers. Elliott Hagedorn, PhD, a researcher in Hematology & Medical Oncology and Associate Member of the Center for Regenerative Medicine (CReM), uses zebrafish to uncover how blood stem cells migrate and take root in the body. By understanding these early-life processes, his lab aims to find ways to enhance stem cell engraftment and shorten recovery after a bone marrow transplant.
HealthCity sat down with Hagedorn to discuss his research and how his lab is innovating solutions for cancer patients.
HealthCity: What inspired you to pursue research in cell and developmental biology?
Elliott Hagedorn, PhD: Growing up, I always liked photography and the process of taking things apart to understand how they worked. My dad had a shop filled with tools, old cars and metal/woodworking machinery. I spent a lot of time there, building and exploring how things work. That same curiosity carried into my academic life—when I started working with fruit flies as an undergraduate, I realized how microscopy and genetics weren’t all that different from the camera and tools I had worked with before.
I was able to capture the beauty of biology through the microscope, and the blend of visual exploration and mechanical curiosity ultimately inspired me to study how blood and cancer cells migrate through tissues and organs. It’s a complex, dynamic process that my research group continues to explore with that same desire to understand how things move, function, and interact.
HC: Why do you use zebrafish to study how cells move?
EH: Zebrafish are native to South Asia but are also a common aquarium fish sold in pet stores. They were adopted as a popular research model, in part because they are hardy and easy to work with. It might seem surprising, but the biology of the fish is remarkably similar to that of humans.
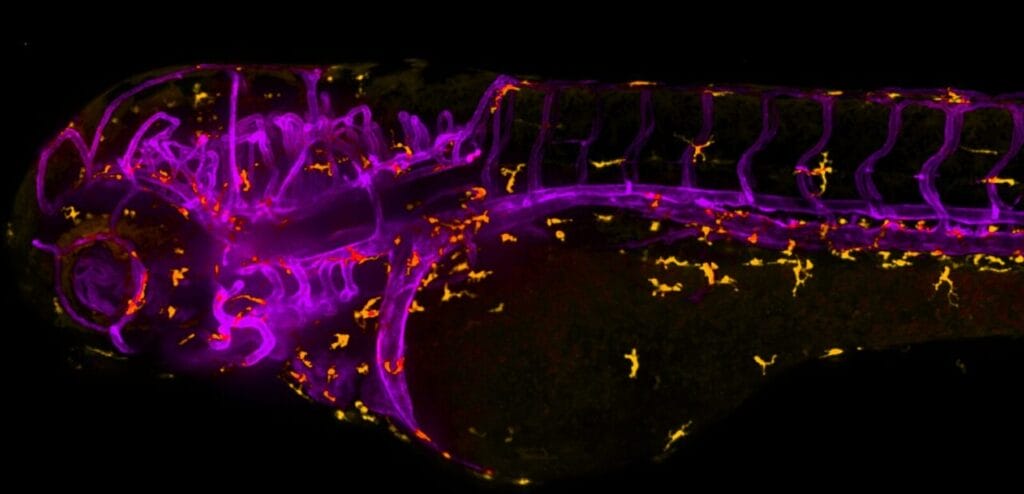
My lab uses zebrafish because their see-through embryos allow for high-resolution live-cell imaging without the need for invasive procedures. We can label specific cells or cellular components using fluorescence and directly observe their dynamics in real time under a microscope. Being able to directly visualize these events as they happen in real time in the zebrafish provides critical insights into cell migration events that are difficult to capture in other model systems like the mouse.
HC: What is the goal of your cellular and developmental biology research?
EH: My group is broadly interested in understanding how cells move in and out of tissues—a process that’s essential for normal development and everyday physiological events, like when immune cells rush to a wound to help it heal.
“By exploring the cellular pathways that guide this kind of cellular movement, we hope our work will ultimately be able to improve the treatment for a range of cancers.”
One area we focus on is the migration of blood stem cells in the context of bone marrow transplants for cancer patients. These transplants can be lifesaving but remain a risky procedure. Patients often undergo intense chemotherapy or radiation to prepare for the transplant, which weakens their immune system and makes them vulnerable to infections. After the transplant, there’s a critical period where the new stem cells need to find their way to the right place in the bone marrow to rebuild the immune system.
Our goal is to find ways to coax the donor blood stem cells to the right location in the recipient’s body more efficiently, so they can rebuild the immune system even faster and reduce the time that the patients are immunocompromised. We are particularly interested in understanding the genetic and cellular mechanisms behind normal cell migration with the idea that we can tweak these pathways to improve transplant outcomes. A key part of this work involves cutting-edge imaging technologies—like spinning disk confocal and light sheet microscopy—that let us capture detailed 3D time-lapse images of cells as they move inside of a living organism.
HC: How does your cell and developmental biology research impact patients?
EH: Although our research is focused on the basic science of how cells move and behave, it has the potential in the long-term to make a real difference for patients and their families. By partnering with physician-scientists who interact directly with patients, we’re working to translate our discoveries into new therapeutic strategies.
Our work has potential implications for cancer therapies beyond bone marrow transplants, such as guiding engineered immune cells—like CAR T-cells—into solid tumors, which is an exciting new frontier for the field. By exploring the cellular pathways that guide this kind of cellular movement, we hope our work will ultimately be able to improve the treatment for a range of cancers.


