Alyssa Tilhou, Boston Medical Center
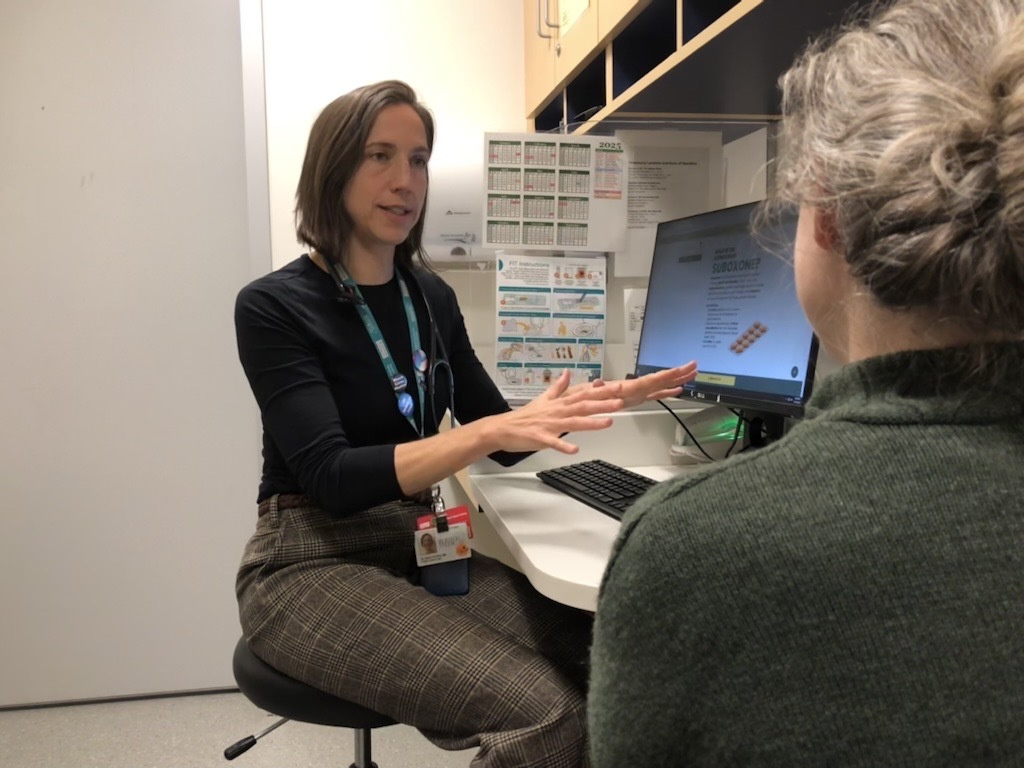
Dr. Alyssa Tilhou in her office at Boston Medical Center.
Guided by her research, Alyssa Tilhou, MD, PhD, is advancing models of care that bring effective opioid use disorder treatment directly into everyday family practice.
Effective family medicine treats individuals not just as patients with medical conditions, but as members of families and communities with unique experiences, values, and environments. For Alyssa Tilhou, MD, PhD, this intersection of individual care and community health drives her goal to understand how care is delivered and how it can be improved in line with what patients need. Her work centers on optimizing treatment for opioid use disorder (OUD) and designing systems that make it easier for patients to engage in and sustain recovery.
HealthCity recently spoke with Dr. Tilhou, who is the Vice Chair for Research at Boston Medical Center (BMC), to discuss how her research could help patients with OUD engage in care in a way that centers patients lived experiences and perspectives.
HealthCity: What inspired you to pursue family medicine research?
Alyssa Tilhou, MD, PhD: I was drawn to family medicine even before medical school. My background was in public health, and I spent a summer in Santiago, Chile, where I was paired with a family doctor in their public health department. Watching her, I saw how deeply connected the delivery of care is to the environments that keep people healthy. I worked in mobile rural clinics across the city and became immersed in the realities of people’s lives and the barriers they face in accessing care.
When I started my first job in rural Wisconsin, I practiced the traditional full-spectrum family medicine model. But the community had a growing need for treatment of OUD. As I began caring for those patients, I found the challenge both humbling and intellectually engaging. I wanted to better understand how to help people achieve their goals for recovery and how to create systems that make it easier to enter and stay in treatment.
“I’m also very interested in aligning research with what actually matters to patients and clinicians. We’re asking both groups about their goals for treatment because by understanding those perspectives, we can make treatment more meaningful for the people receiving it. “
Alyssa Tilhou, MD, PhD, Vice Chair for Research at BMC
That led me to pursue an addiction medicine fellowship and, ultimately, research in this area. My work now focuses on bringing evidence-based interventions for addiction to patients and understanding where implementation breaks down in real-world settings.
HC: What is the goal of your family medicine research?
AT: I’m a health services researcher, which means I study the delivery of care — describing what kinds of care people receive, who receives it, and what the outcomes are. Much of this involves analyzing large quantitative datasets, including administrative claims data and clinical information from electronic health records. These data help us estimate relationships between early aspects of care — such as like patient demographics, medication patterns, or co-occurring conditions — and long-term treatment outcomes.
But what’s often missing in those data are the nuances of patients’ lived experiences. My goal is to bridge that gap by studying the long-term picture of treatment-seeking at the individual level and understanding how people come into and out of care over time. Those transitions are critical moments. If we can identify specific inflection points, or times when people are most likely to engage or disengage from care, we can design interventions to make those moments more effective.

A key part of my work looks at optimizing patient engagement in treatment for OUD. For example, we know that being on medications for OUD over the long term helps people achieve stability and work toward other life goals. My research explores what factors help people stay on medication consistently and successfully.
I’m also very interested in aligning research with what actually matters to patients and clinicians. We’re asking both groups about their goals for treatment because by understanding those perspectives, we can make treatment more meaningful for the people receiving it.
HC: How does your addiction and family medicine research impact patients?
AT: At the heart of my research is the belief that we need to aim for the outcomes that matter most to patients. It isn’t enough to develop interventions that work in controlled research settings if patients can’t access them in real-world settings or if the benefits aren’t a priority to patients. If we don’t ask people what they value, why they think certain treatments are working, or what success looks like to them, we risk targeting the wrong goals. That’s why a key part of my current work involves qualitative interviews, or listening directly to patients. So that when we design interventions, they’re aligned with what people actually care about.
For example, most people living with substance use disorder don’t want to overdose or be caught in a cycle where their drug use interferes with other things they care about. If my research helps people stay on medications for OUD, then it can directly reduce overdose risk and open the door to broader health and life improvements.
At the heart of my research is the belief that we need to aim for the outcomes that matter most to patients. It isn’t enough to develop interventions that work in controlled research settings if patients can’t access them in real-world settings or if the benefits aren’t a priority to patients.
Alyssa Tilhou, MD, PhD, Vice Chair for Research at BMC
In family medicine, we rarely see patients with just one health problem. When someone achieves stability in their substance use, it often becomes easier for them to engage in other aspects of care, such as preventive health screenings, managing chronic conditions, or addressing mental health needs. As a family doctor, I’ve seen how treatment with medications like buprenorphine can create opportunities to deliver more comprehensive care.
Ultimately, my goal is to design systems and strategies that make it easier for people to achieve their treatment goals and to build healthcare environments that truly support whole-person health. Patients are our greatest source of insight, since they understand their challenges and needs better than anyone. When we ground our research in their experiences and perspectives, we not only build trust but also create interventions that are more effective and meaningful for patients and their families.
This interview has been edited and condensed for length and clarity.


