Answering the Most Important Questions About Mpox
August 23, 2022
By Cassandra M. Pierre, MD, MPH, By Glory Ruiz, MD, By Samantha Johnson
Boston Globe, Getty Images
Misinformation and misconceptions about mpox are rampant, but three experts are here to tell the facts from the fiction.
On Friday August 5, the U.S. declared mpox, previously known as monkeypox, a public health emergency. In response, Cassandra Pierre, MD, MPH, infectious disease physician, medical director of public health programs and the associate hospital epidemiologist at Boston Medical Center (BMC); Glory Ruiz, MD, the director of public health programs at BMC; and Samantha Johnson, the operations manager of public health outreach, education and prevention sat down for a roundtable discussion about mpox, common misconceptions, prevention, the mpox vaccine, and more. Marquis Jamison, the program manager of HIV/STI prevention and screening contributed information to this discussion.
How does mpox misinformation spread?
Glory Ruiz, MD: There is a general, pervasive fear and concern that you can get mpox from congregate settings, such as schools, college dorms, prisons, and public places like gyms, retail stores, and pools.
HeathCity: Is there confusion because of COVID-19? Are people conflating the two, particularly around how mpox is spread?
Samantha Johnson: There’s a lot of miscommunication about community exposure, predominately because patients are getting their information on social media. For instance, we have retail workers and food service workers calling us to say that someone they work with has been exposed to mpox and they feel panicked. Keeping in mind their experiences during the COVID-19 pandemic, that can lead to a feeling of mass panic.
Cassandra Pierre, MD, MPH: These are all the things that people were also worried about with COVID-19. But it’s very important not to conflate the two. They are different diseases. Mpox is an infection spread by prolonged close contact. With mpox, should people be afraid to go to the grocery store, like many were at the onset of the COVID-19 pandemic? The answer is clearly no.
SJ: Again, a lot of this misinformation is coming out of social media. For example, I watched a TikTok with a woman saying her baby was born with mpox.
CP: To be clear, that is extremely unlikely.
SJ: Yes, based on my experience, I can see that the patient is presenting with infant acne. But for a lot of patients who are seeing information like this, it becomes difficult to parse what’s true.
“I see [mpox] misinformation that conflates the risk community exposure to COVID-19, which is typically shared in good faith by people who want to protect their friends and family members.”
I see misinformation that conflates the risk community exposure to COVID-19, which is typically shared in good faith by people who want to protect their friends and family members. In another example, I spoke with a man who feared for his elderly mother. Thinking in a COVID mindset, he had decided to lock himself in a room as a quarantine every time he visited Provincetown, trying to be as conscious as possible about putting his mother at risk. Again, based on what we know about the way mpox is transmitted, we don’t see a need for lockdowns and quarantining unless you’ve had a credible exposure.
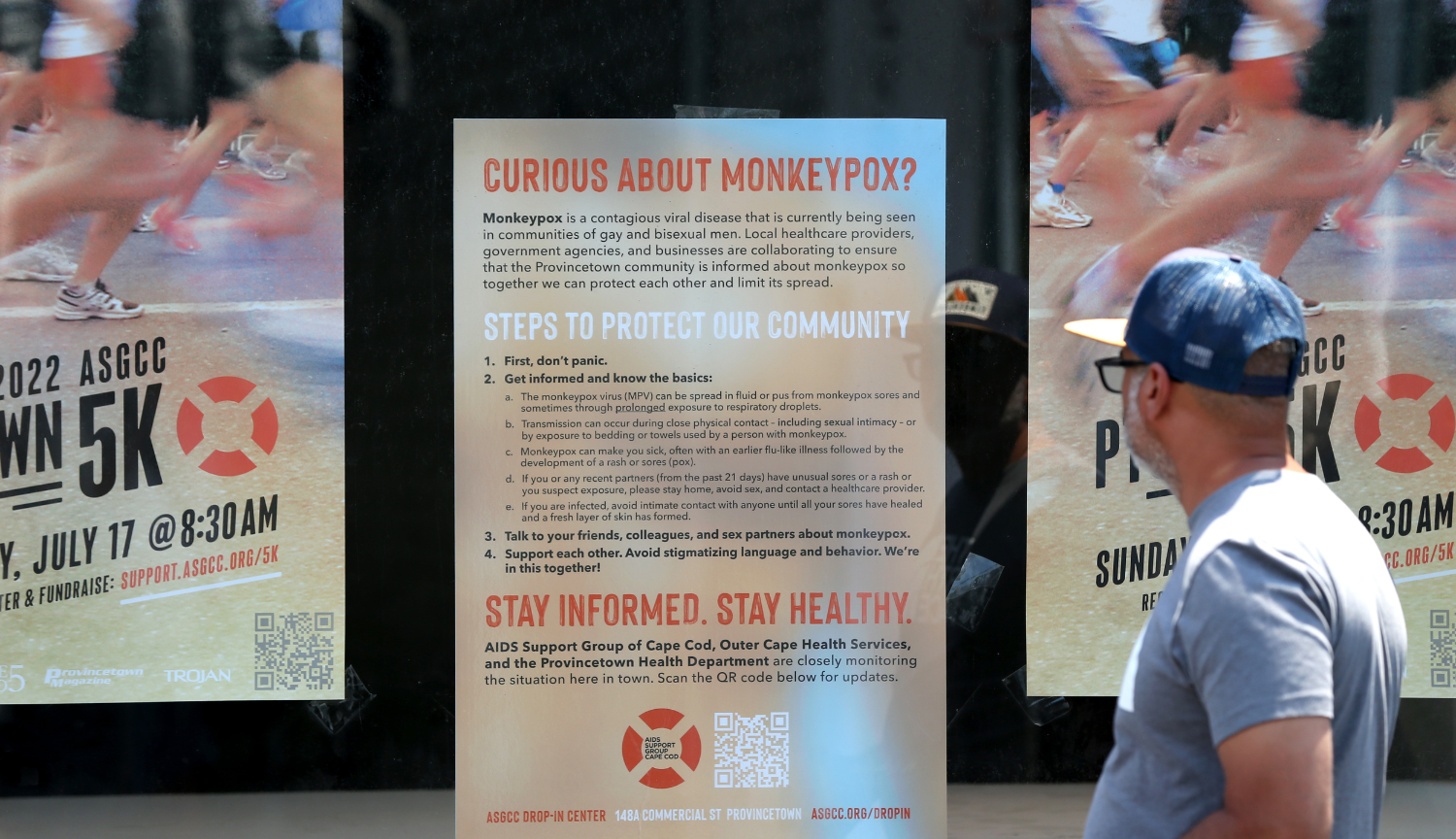
[Editor’s note: Provincetown is a popular Cape Cod vacation spot for LGBTQ+ visitors. While currently largely affecting men who have sex with men, mpox is neither a sexually transmitted infection nor does it only affect MSM.]
Can you get mpox from a pool, retail store, school, or other congregate settings?
HC: Should we go through these fears and debunk misinformation one by one? Because it’s summer, let’s start with pools.
SJ: We’re getting tons of questions like, ‘Can I get mpox from swimming in the same pool as somebody that has mpox?’
GR: No. Not just from swimming in the same water.
HC: How about for kids in school?
CP: To reiterate, mpox is spread primarily by prolonged close contact, face-to-face by a period of approximately three hours or skin-to-skin with infected areas. Given what we know about mpox, those brief interactions during school is not the same as hugging people all day. Even at recess where kids are playing and tackling — those are brief interactions and not an immediate cause for concern.
HC: Retail stores?
CP: Retail environments are a valid concern. Let’s talk about it.
Take this exaggerated case: Someone who had mpox could theoretically rub a dollar bill on an infected lesion, by accident, and then hand it to you. You’ve still only come into contact with this bill for a very short duration, and the infectious threshold has not been met. You have very low risk of getting mpox.
HC: How about in retail dressing rooms, trying on clothes?
CP: At this point, I would not be worried about trying on clothes. In this case, like in all cases, it’s about appropriate preventative measures and situational awareness.
GR: There’s also fear about the risk on public transit, college dorms, and the like.
CP: That threshold of prolonged face-to-face or skin-to-skin contact is unlikely to be there. Again, situational awareness is really important.
How can people protect themselves from mpox?
CP: Going back to trying on clothes in a retail environment, you can protect yourself right away. It’s true that you may not know anything about the person before you how tried on that piece of clothing, and you may not be sure if the store launders clothes after trying on — though you can ask the latter. I’d advise just using situational awareness to weigh your risk, and if you do try on the clothes, sanitize your hands before and after and ensure the sensitive areas of your body are covered. Wear underwear and a bra.
HC: Hand sanitizer, that is one thing that does seem to intersect with COVID-19.
CP: Good hand hygiene is so important overall. If you’re a retail worker, it’s absolutely a way to reduce your risk — and your anxiety — by washing and sanitizing before, after, and during your retail shift. That should be sufficient.
HC: Would you recommend gloves at any point?
CP: I’m not recommending gloves, but there are people who may decide they want to wear them because it makes them feel more comfortable, and that’s fine. Hand hygiene, even if you do wear gloves, is way more important.
That’s the same for children going to school and most congregate settings.
HC: What about people who want to continue being sexually active? How can they prevent mpox and stop the spread?
“Facebook, TikTok, and other social platform algorithms are pushing you toward misinformation, a more robust presence from the public health community on these platforms could better the chances of getting accurate information.”
CP: Sexually active people can protect themselves against mpox in a few ways. Start by initiating open, honest, and non-stigmatizing conversations with current and potential partners about recent symptoms or new rashes, risk tolerance, and even mpox vaccination status. Be aware of changes in your or your partners’ health, which includes the presence of any new rashes/lesions and avoid sexual or intimate contact with individuals who have new skin lesions or feel unwell. If possible, temporarily reduce the number of new sexual partners or create a temporary closed network of sexual partners. Remember the basics: wear condoms when possible and wash hands frequently. Get vaccinated and encourage your partner(s) and friends to get vaccinated if they’re eligible.
What is health systems’ role in countering misinformation?
SJ: Within the healthcare community itself, social media has the possibility to have a really positive impact on dissuading this information. Unfortunately, a lot of the public health system does not have a very active social media presence. Because information is spread online now, with Facebook, TikTok, and other social platform algorithms are pushing you toward misinformation, a more robust presence from the public health community on these platforms could better the chances of getting accurate information.
CP: We’ve said this throughout COVID-19, as well, that public health needs a better platform online, as well as community leaders that are trusted. As much as possible, it’s important to use the networks developed during COVID-19 to continue to empower community leaders who may not necessarily see themselves as being important for mpox, but whose voice would be really important to ensure that everyone knows what the actual risk is and are protecting themselves. There’s lots of fear generally, regardless of whether you perceive yourself to be at higher risk or not.
GR: At Boston Medical Center Health System, specifically, we’re not reinventing the wheel. We know we have the finger on the pulse of vulnerable communities. We know we have a community presence that was further solidified with our robust COVID-19 community vaccination and information initiatives. That’s where we can leverage our trust-building for impact.
This is part two of a three-part mpox discussion. Click here for part one, and stay tuned for part three, which focuses on mpox and healthcare workers.


