COVID-19's "Alarming" Effect on HIV Outbreaks Among People Who Inject Drugs
February 9, 2021
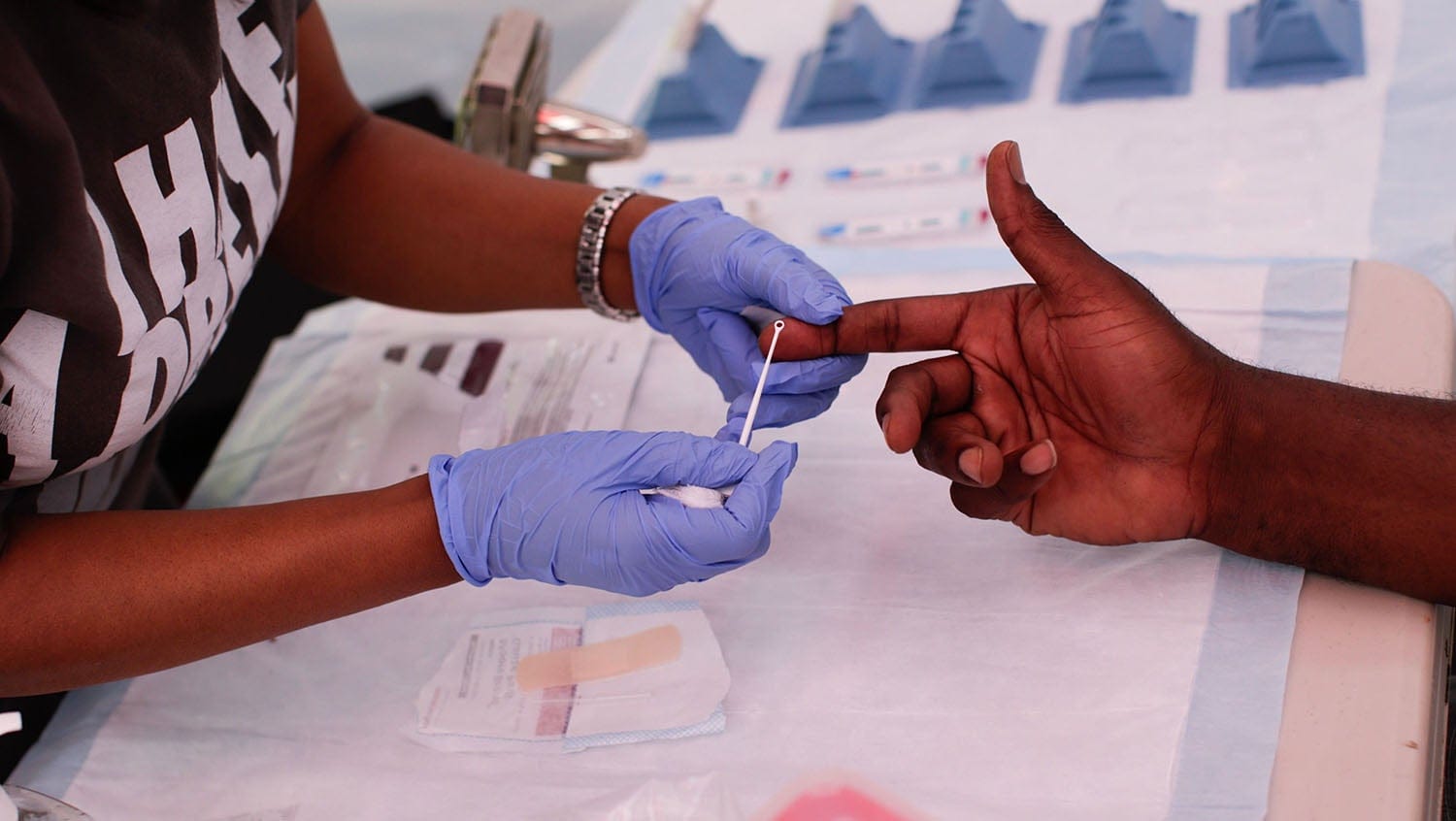
Getty Images
The HIV outbreak impacting people who inject drugs has only escalated during the pandemic — here's how it's being addressed.
Prior to the COVID-19 pandemic, there were several HIV outbreaks happening in various locations in the United States among people who inject drugs (PWID). Studies published in 2018 and 2019 demonstrated that injection opioids, including fentanyl, and methamphetamines were driving this increase in HIV cases in Seattle and Massachusetts, respectively.
Moreover, existing treatment and harm reduction services, including low-barrier access to HIV testing and treatment, needle exchanges and condom distribution, and HIV pre-exposure prophylaxis (PrEP), were not proving adequate to eliminate HIV transmission among PWID.
As the pandemic led to abrupt changes and restrictions within society — affecting virtually every area within the healthcare system — providers who treat PWID became concerned about the unintended consequences that these changes would have on HIV cases.
Jessica Taylor, MD, the medical director of Faster Paths to Treatment, Boston Medical Center’s substance use disorder urgent care program, recently looked at how the ongoing COVID-19 pandemic has been impacting patient access to HIV testing and preventive services in her clinic and others throughout the hospital.
What she found was not surprising, she said, but alarming, and it speaks to the urgency of providing HIV prevention services when caring for individuals with substance use disorders.
HeathCity: Can you tell me what you were seeing in Faster Paths to Treatment in terms of volume and HIV testing rates in 2019, prior to the COVID-19 pandemic?
Jessica Taylor, MD: Prior to the COVID-19 pandemic, Faster Paths saw just more than 600 patients per year, or about 50 patients per month. We offer HIV testing to all new patients on an opt-out basis — meaning that we default to testing unless a patient does not want to test — and we typically ran 35 screening HIV tests per month before the pandemic.
HC: You just recently published a paper in the Journal of Substance Abuse Treatment that showed a tremendous decrease in the number of HIV tests performed at BMC during the first weeks of the pandemic. What did those results demonstrate to you about dealing with an HIV outbreak among PWID during a pandemic?
JT: The drop-off in HIV testing volume really alarmed us. During the first 45 days of modified operations for the pandemic, in-person visits and HIV testing volume in Faster Paths dropped by half. Across BMC, HIV testing in ambulatory clinics dropped by more than 90%.
But we knew that even though fewer people were coming into the medical center to undergo testing, the COVID-19 pandemic did not eliminate — and in many circumstances may have increased — HIV transmission among people at highest risk.
We had an active HIV outbreak among PWID in Boston even before the pandemic. When COVID-19 infections started to ramp up, organizations that serve PWID had to rapidly evolve to comply with infection prevention recommendations, which led to service interruptions. Simultaneously, many people who had the opportunity to leave the city did so, and many others who were no longer able to stay with family or friends came to Boston for the first time.
The overall effect was that many PWID were separated from medications for OUD, HIV prevention, and other harm reduction services. We believe these service interruptions contributed to ongoing high HIV transmission among PWID, which unfortunately is what our data showed. By June 2020, the number of new HIV infections in PWID at our institution was already double the annual average from 2018 to 2019.
HC: Why was it important for you to keep Faster Paths open for in-person visits during the pandemic?
JT: On-demand access is a key principle in a bridge clinic, and many of our patients depend on the flexibility of being able to see us on a walk-in basis. Many of our patients also lack phones and technology as well as private spaces to hold telemedicine visits with providers. We were worried that, if we shifted entirely to telemedicine, these patients would be excluded from care and would be at still higher risk of complications such as overdose and HIV infection.
HC: As you saw the dramatic decrease in the number of HIV tests performed at BMC during the first part of 2020, what strategies did you put into place to help bring those numbers up?
JT: We focused primarily on educating providers about the ongoing HIV outbreak and the importance of coordinating testing, even if it did not happen at the same time as the visit. For example, when patients had telemedicine visits, we encouraged providers to put lab orders in so that patients could walk in to leave a blood sample. Over time, this has become very routine, but it was a new way to practice for us as we adjusted to telemedicine.
We also encouraged providers to help patients make a plan for testing even if they did not want to come into the medical center. For example, several local service providers offered street-based rapid HIV testing. Although the lab-based 4th generation HIV antigen/antibody test is the best test in early infection, a rapid test is much, much better than no test at all.
Finally, we have collaborated with our inpatient colleagues to make sure we take advantage of other touch points with the health system, such as ED visits and hospital admissions, to screen and offer HIV prevention services like pre- and post-exposure prophylaxis (PrEP and PEP).
HC: And how about getting patients at high risk for HIV to consider PrEP or PEP?
JT: This is so important. PrEP and PEP involve using HIV medications to prevent HIV infection in people at high risk due to injection and/or sexual practices.
If someone has had a very recent, high-risk exposure (typically within the past 3 days), we offer PEP, which is a 28-day course of 3 HIV medications used to prevent HIV infection. In cases in which patients have not had a very recent exposure, we recommend PrEP, which involves taking 2 HIV medications in a single pill once a day to prevent HIV infection.
PrEP works very well; the problem is that few PWID are offered PrEP alongside other HIV prevention options. Condoms, syringe services, medications for OUD, and low-barrier HIV testing and treatment are all important interventions — and they have not been enough to stop the HIV outbreak in PWID. PWID deserve access to every HIV prevention tool we have available, including PEP and PrEP.
HC: What are the biggest takeaways? How can addiction medicine providers and beyond help prevent HIV in PWID, during the COVID-19 pandemic and beyond?
JT: The biggest takeaway is that the HIV outbreak impacting PWID has not slowed down for COVID-19. In fact, HIV transmission continues to escalate. Whether we are caring for PWID as an addiction medicine team, a hospital medicine team, in the emergency department or in the community, we may be the only point of contact that someone has with the medical system, and it is critical we take that opportunity to address HIV prevention.
Specific steps can include distributing higher quantities of condoms and safer injection equipment; offering on-demand HIV testing and access to rapid HIV testing for people who do not want a blood draw; offering low-barrier medication treatment for OUD; and offering HIV PrEP and PEP.
Partnering with non-clinical community-based service providers is also critical, especially in the era of telemedicine, which has opened up new opportunities to connect with patients who are not physically at the medical center.


