A New Shared Decision-Making Tool Empowers Patients in Fibroids Management
July 25, 2024

Getty Images
"We've gotten positive feedback so far from patients about their experience with the tool being a very humanizing approach and feeling like they were being heard," Dr. Kelly Treder, who helped develop the tool.
Four out of five people with uteruses will develop uterine fibroids by the age of 50, but not all women are affected in the same way by these benign uterine growths. Black women are diagnosed younger and more frequently than white women, and they often have worse fibroids and more severe symptoms, including pelvic pain, heavy bleeding, and infertility.
Dismantling this disparity is what guides the patient-centered approach at the Fibroid Center at Boston Medical Center (BMC). The team knows that just as patients experience fibroids differently, they also want and need different treatments.
“Black people with fibroids report that their feelings and symptoms are dismissed, and that they aren’t given all of their management options,” explains gynecologist Nyia Noel, MD, MPH, who founded the center in 2021. “Often, even though they would much rather have a non-surgical option, they’re counseled toward a hysterectomy, complete removal of the uterus.”
With funding from the Health Equity Accelerator through the fall of 2025, the Fibroid Center at BMC developed and is piloting a shared decision-making tool. The tool aims to help providers approach fibroids care through a health equity lens.
“Our hope is that if we give providers a tool that requires them to ask about a patient’s priorities and preferences, it will be easier for them to deliver patient-centered care and harder to allow their unconscious bias to seep in,” says gynecologist Kelly Treder, MD, MPH, who helped lead the development of the tool. “Our goal with these types of tools is that they’re strategies to combat racism in medicine, because we have struggled to find ways to address that on a clinical care level.”
We caught up with Noel, Treder, and program management specialist Emma Forbes, MPH, to discuss their progress in rolling out the shared decision-making tool.
HealthCity: Can you describe the fibroids management tool and explain how it’s being used?
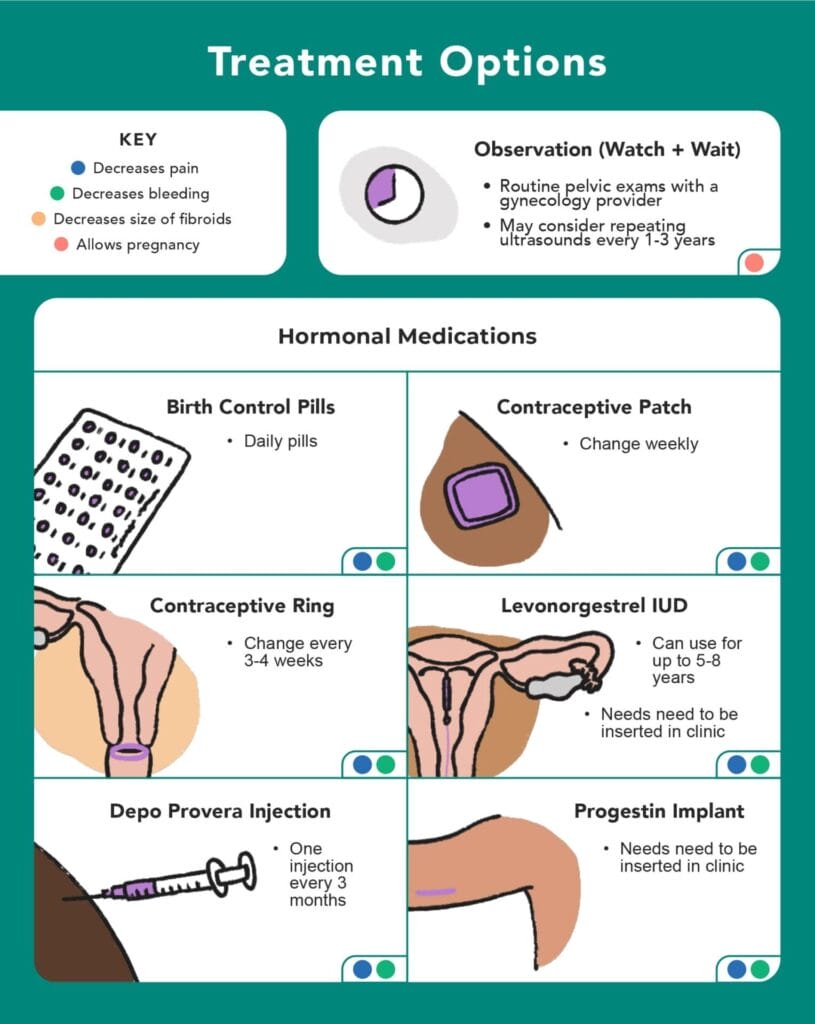
Nyia Noel, MD, MPH: It’s a simple, tangible worksheet that teaches patients about their bodies and all their options for fibroids management. We also offer providers strategies for how to walk through it and engage with a patient in a conversation about their goals and their management for fibroids. The worksheet was created in partnership with a graphic designer, so it has beautiful artwork, and is inclusive and readable.
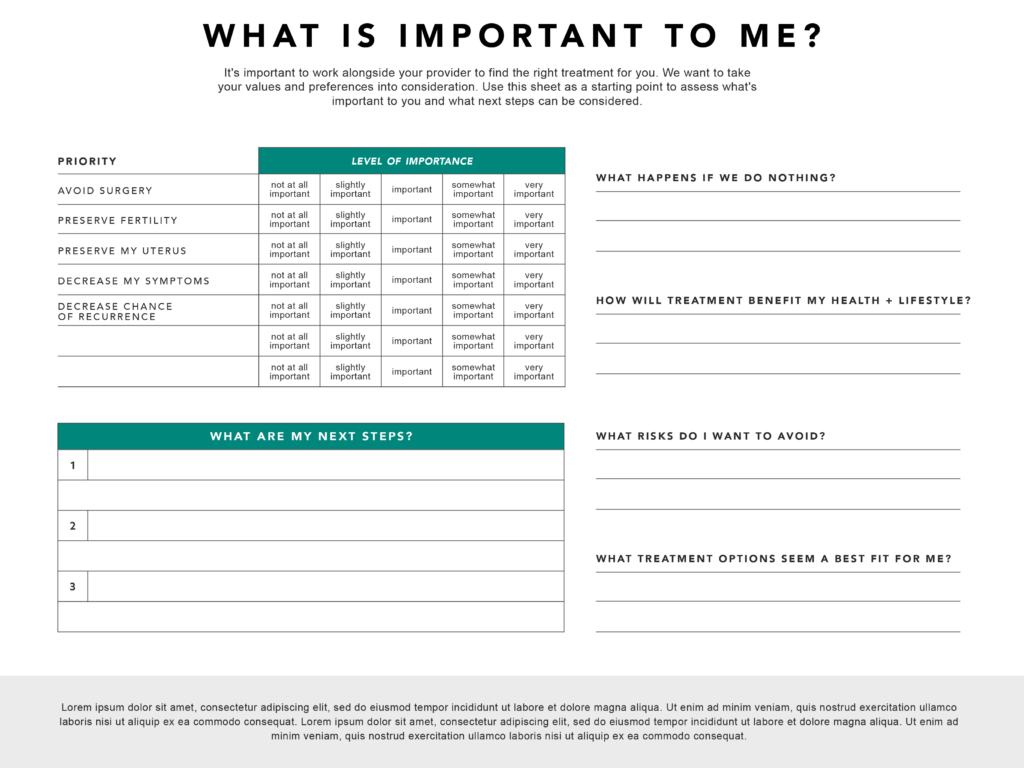
Emma Forbes, MPH: We’re currently piloting the tool in outpatient gynecology clinic visits, where providers familiarize themselves with the worksheet and then move through the questions together with the patient. They then take a picture of the patient’s Likert scale for their chart, and the patient takes the worksheet home with them.
HC: Why is shared decision-making important in fibroid care?
Kelly Treder, MD, MPH: Shared decision-making is especially important in gynecology because patients have all sorts of values and other cultural notions tied up in their reproductive health. Some clinicians take a simplistic view that reproduction is the key role of the uterus, and that once you’re done having kids, it’s no longer necessary. But for some people, reproduction isn’t the ultimate focus or end goal, which speaks to the need for individualization. With shared decision-making, two different types of experts — patients and providers — come together and make a plan that is rooted in the patient’s values.
NN: Fibroid management is an appropriate sphere for shared decision-making because fibroids are benign, they’re not cancer. The management of fibroids is totally dependent on a person’s individual symptoms, their desires for treatment, and their values around certain treatments.
HC: Do you have any initial feedback from providers?
EF: We’re in the process of surveying 200 users and interviewing 30 patients and 15 providers about their experience with the tool. So far, we’ve had an overwhelmingly positive reaction to the tool from both patients and providers. Some providers are looking for it to be a little more tailored to their practice, so we’re thinking about that, as we want this tool to be as ubiquitous and relevant as possible, using the latest science on fibroid care.
KT: As providers, we have maybe 20 minutes with patients to explain their diagnosis and all their treatment options. If you consider that some patients have interpreters or haven’t interacted frequently with the healthcare system and it’s challenging to do in a way that’s not confusing. This tool allows providers to have efficient but thorough conversations with patients.
I think we’re going to learn a lot of new ideas through this process as to how to best use it in practice. We want to eventually roll the tool out to community health centers and other hospitals with instructions on how to use it in a way that’s effective and efficient in clinic.
HC: And what are patients saying so far?
KT: As we review initial transcripts, we’re not surprised to see that many people with fibroids have been told their best option is to have a hysterectomy in previous clinical encounters. A complete removal of the uterus can work well to treat fibroids definitively if the patient is done with childbearing, but there are some patients that ascribe a value to their uterus that’s completely outside of reproduction. So, even if the uterus is causing symptoms or problems, they really don’t feel a total hysterectomy is a treatment plan that aligns with the value they hold for their uterus and their body. We’ve gotten positive feedback so far from patients about their experience with the tool being a very humanizing approach and feeling like they were being heard.
EF: In this early stage, we’re seeing increased self-efficacy. Patients have said that the tool made them feel like the decision was theirs. I’ve had a couple of conversations with patients who previously experienced racism in the fibroid and medical space. These experiences, while unfortunately not anything new, have confirmed why we’re doing this study.
*This interview has been edited and condensed for clarity and length.


