
Boston Medical Center
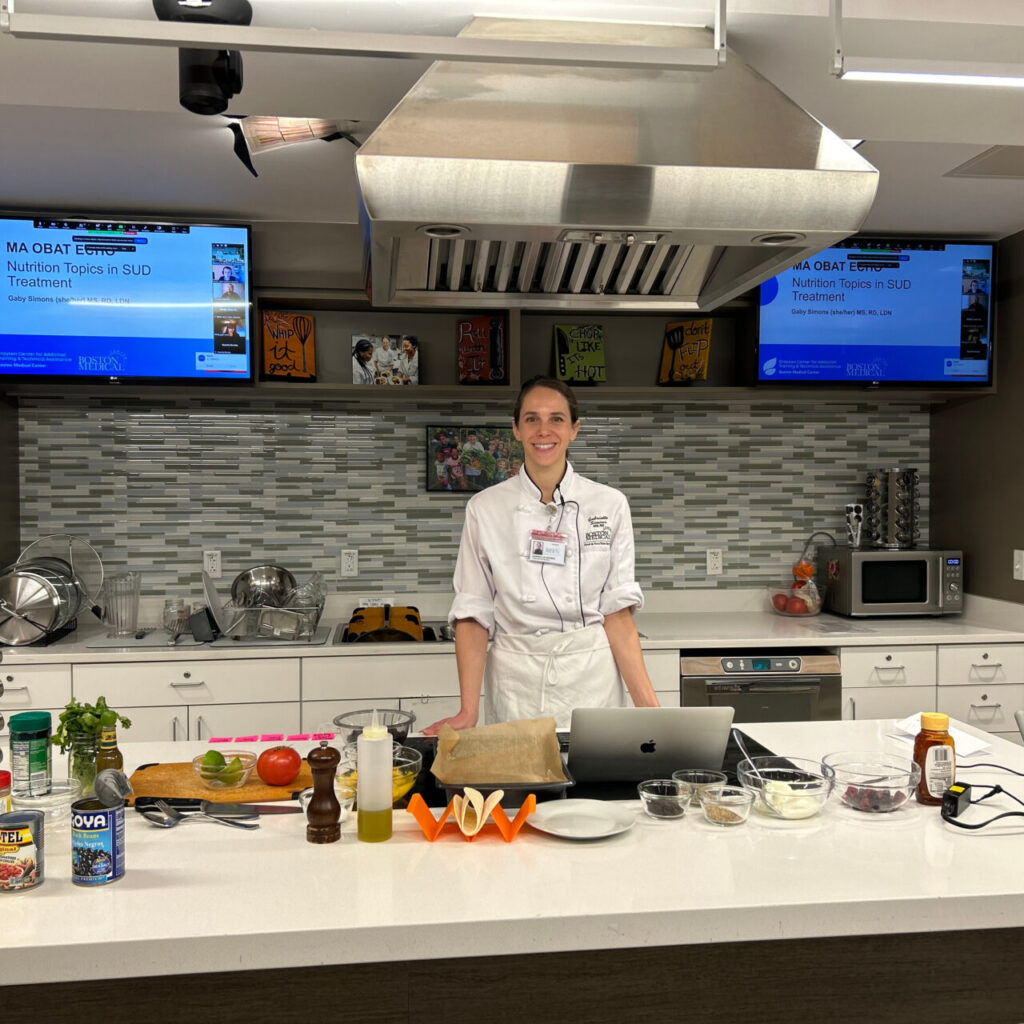
A window into Boston Medical Center's Teaching Kitchen
BMC’s Teaching Kitchen offers culturally relevant, accessible, and tasty food to supplement care plans for a variety of chronic conditions, including diabetes.
In 2023, the American Heart Association (AHA) advocated for incorporating healthy foods as part of patient care, particularly for patients with chronic illness, including diabetes. While Massachusetts has one of the lowest rates of diabetes in the country — contributing only .0015% to the national total — diabetes rates remain disproportionately higher among historically underrepresented patient populations on the state and national level. Boston Medical Center (BMC) has responded to this care gap by adding diabetes-specific cooking classes to its Teaching Kitchen program offerings.
“Food allows us to communicate in a bigger way where the lessons learned in class can translate not only into a person improving their health, but their families and communities improving their health as well.” says Mara Garwood RD, a registered dietitian in BMC’s Endocrinology Department and a certified diabetes educator in the Teaching Kitchen.
A history of the Teaching Kitchen
BMC’s Nourishing Our Community Program is a national model in prioritizing healthy food as an essential aspect of healthcare. The program encompasses three prongs: the Preventive Food Pantry (the first in-hospital food pantry in the country), the Teaching Kitchen, and the two Rooftop Farms, Power Plant Farm and Newmarket Farm.
The Teaching Kitchen offers interactive patient-centric nutrition education through virtual and in-person classes. From its inception in 2008, the Teaching Kitchen has blossomed into a well-attended program, serving an average of 150 patients per month, through classes devoted to specific diagnoses or groups, including Food Explorers for kids and their families, Cancer and Sickle Cell Support, and Diabetes Essentials.
Through an array of programming, the kitchen serves as an expansion of the examination room. In close collaboration with BMC-affiliated clinics and local community groups, providers are welcome to bring individual patients or patient groups with similar nutritional needs and goals to the kitchen through means of a shared medical appointment focused on specific health issues. The program also offers community classes focused on general wellness.
Teaching for a medically tailored plate
In 2019, the Department of Endocrinology’s Clinical Diabetes Program expanded its educational programming under the umbrella of “The Conversation Map for Diabetes Education” in a class called Comprehensive Diabetes Education. This class aims to provide diabetes self-care empowerment, education, and skills to help reduce the risk of complications associated with the disease. In 2025, the Department of Endocrinology’s Clinical Diabetes Program announced two new classes titled, Continuous Glucose Monitoring and Cooking for Diabetes Advanced Nutrition. The latter class is a collaboration with BMC’s Teaching Kitchen.
“The diabetes Teaching Kitchen classes are a space to understand how food impacts our health, our blood sugar, and how it can be enjoyed in a way that helps us reach our health goals,” says Garwood, “The goal is not to focus on what we can’t eat, but what we can eat and enjoy.”
Teaching Kitchen staff, Diabetes Education staff, and outpatient providers co-create each class to ensure a medically tailored plate. The classes are typically two hours long and delivered in a two-part format. First, a Diabetes Education team member dives deep into the class’s theme—for example, one class may focus on glucose monitoring. Second, the Teaching Kitchen team conducts a hands-on cooking demonstration.
“Food allows us to communicate in a bigger way where the lessons learned in class can translate not only into a person improving their health, but their families and communities improving their health as well.”
Mara Garwood RD, registered dietitian, BMC Endocrinology Department
For example, in one class, called “Demystifying the role of carbohydrates, continuous glucose monitoring,” Teaching Kitchen Manager Gabrielle Simons MS, RDN, LDN, shares a reimagined take on traditional spaghetti and meatballs. Taking into account a full range of dietary needs, she demonstrates how to use whole wheat noodles and zucchini noodles, or zoodles — a low glycemic option and substitute for people with gluten intolerances — accompanied by two meatballs options, turkey or tempeh for vegetarians, all dressed with a basil and tomato pesto dressing.
“Our classes are not cookie cutter,” says Simons, who manages the cooking part of class.
Mindful of each groups’ specific needs and preferences, the curriculum is designed to be adjusted class over class, making each class a one-of-a-kind experience.
A culturally tailored plate that matches lifestyles
The Teaching Kitchen strives to meet patients where they are, not only in their journey with diabetes but also where they are in life.
“We point people toward techniques, ideas, and methods that are not only relevant to their specific nutritional needs, but to their preferences and equipment, monetary, and time constraints,” says Simons.
The best way to support patients in a lasting way, Simons says, is to make food that they can make at home. And what home looks like is different for everyone.
“We want to create a program that is adaptable for whoever comes to our class. This could be someone who’s never cooked anything before or someone who’s cooked a full feast for their family. It could be someone who cooks for one or someone who cooks for a household,” adds Garwood. “We want to open up a new idea of how to incorporate healthy foods without breaking the bank and without pushing any new skills that patients are not ready to learn.”
The Teaching Kitchen strives to deliver culturally relevant curriculum, as well.
“We make a point to acknowledge that foods from all over the world are a part of healthy eating patterns.” says Simmons.
The diverse menu also allows for people to be introduced to a new technique, cuisine, or ingredient that they may not have considered. It’s all possible through shared knowledge in the group.
“We have people from various backgrounds and different palettes, and when we all try the same dish, it opens the door to similarity and common ground,” says Garwood.
Food tastes better with company
In addition to the important medical and cooking skills learning, the communal aspect is just as important. The classes facilitate connection through shared medical appointments with people who have similar medical needs and lived experiences.
“Our diabetes management classes are great opportunities for people to learn from each other because, while it is a very personal condition, patients might have similar hiccups or successes.” That relatability factor Garwood says, “allows for people to feel validated and seen within their personal journey with diabetes.”
Over time, the Teaching Kitchen has received an overwhelming amount of positive patient feedback regarding the social aspect of class — especially in the diabetes classes. As a result, the Teaching Kitchen, in collaboration with the department of Family Medicine and Integrated Behavioral Health, created the Diabetes Support Group. The group is co-facilitated by a social worker, nurse practitioner, and dietitian as a post-educational series for patients who want to receive ongoing support. It emphasizes the co-occurrence of depression and diabetes, addressing another aspect of health.
How the Teaching Kitchen fits into a larger ecosystem of holistic care
Recognizing that the Teaching Kitchen is a part of a larger ecosystem of care, educators like Simons and Garwood weave BMC-affiliated resources into class when appropriate.
For example, Simons makes a special note when ingredients in a recipe come from the Preventative Food Pantry. She hopes it helps normalize and de-stigmatize use of the pantry for people who need it.
Other resources that have surfaced in conversation are elder services or support groups like the Diabetes Support Group for continuous care.
“To me, success looks like coordinating with other clinics so we can create a community for patients who are otherwise feeling abandoned or lonely within their diabetes care.” Garwood says.


