Pandemic Restrictions Create a Reduction in Hepatitis C Virus Testing and Treatment
January 20, 2021
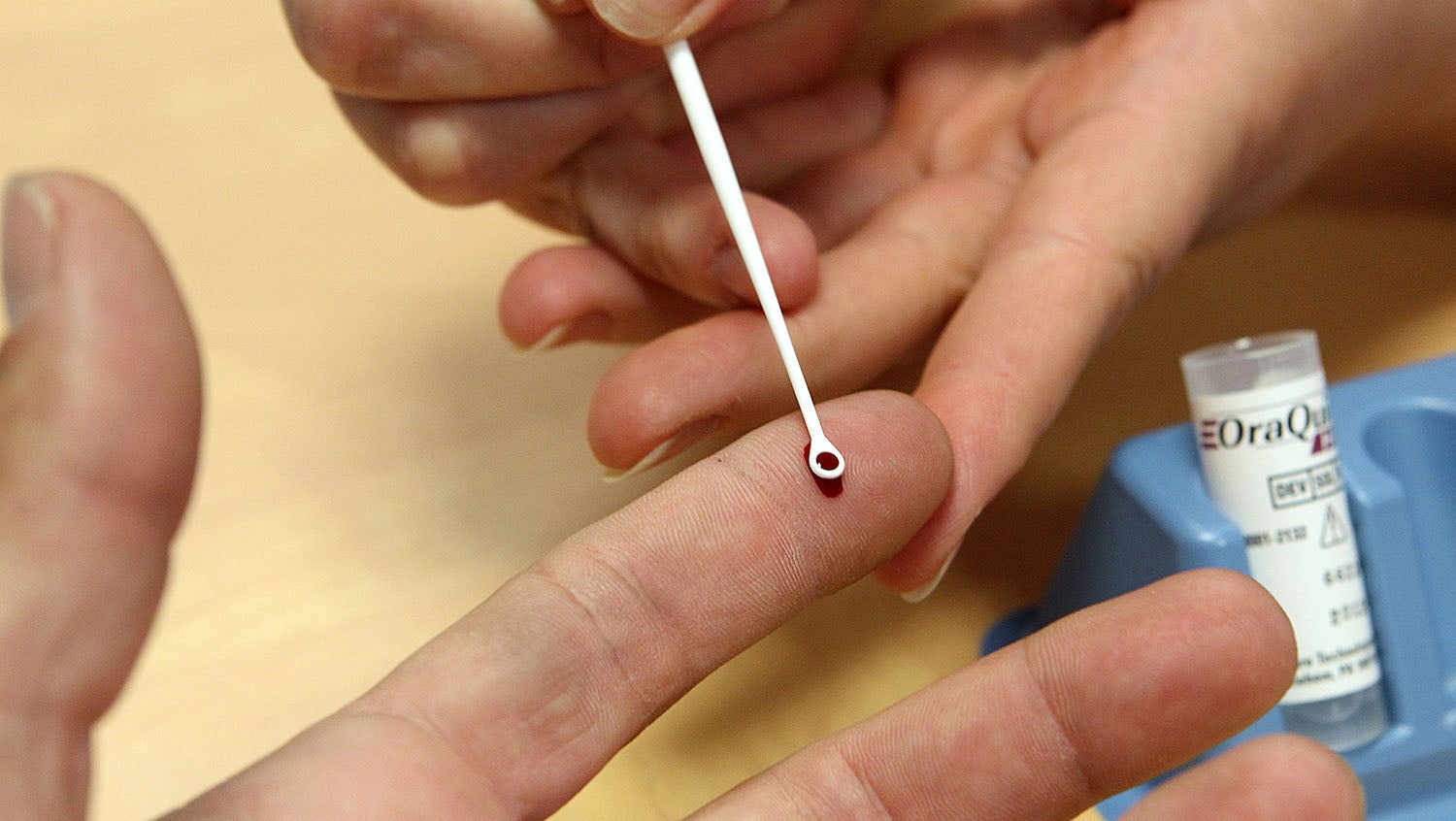
Getty Images
The impact of such a significant decrease in HCV testing and treatment affects both the individual patients and public health as a whole.
During the initial surge of COVID-19, mitigation efforts were put in place at hospitals and medical institutions across the U.S. to protect hospital capacities and prevent transmission among healthcare workers and patients. This meant limiting the number of in-person, outpatient visits. But, these efforts to quell the spread of COVID-19 had a detrimental impact on in-person preventive care. This includes the testing, diagnosis, and treatment of hepatitis C, an easily-transmissible, severe liver infection commonly spread through contact with contaminated blood.
Elissa Perkins, MD, MPH, DTMH, emergency medicine physician at Boston Medical Center and vice-chair of research in the emergency department, highlights new research that showcases this significant impact that COVID-19 restrictions had on testing rates, while offering insight on the importance of hepatitis C diagnosis for both individuals and public health.

Elissa Perkins, MD, MPH, DTMH
“Hepatitis C is a tremendous challenge, especially in communities with a high prevalence of injection drug use. For a number of years, hospital-wide testing programs have been available to ensure that we are recognizing this disease in patients because it’s treatable.
Hepatitis C is one of the leading causes of liver-related deaths nationwide, and it causes thousands of deaths every year in the U.S. It is estimated that there are approximately 3.5 million people that are living with the hepatitis C virus — but most are unaware of their infection. This is because it can take a number of years before symptoms show, including swelling in the body, jaundice, and issues with memory or cognitive function. But, if left untreated, hepatitis C can be fatal. It’s critical that healthcare providers are diligent in recognizing and diagnosing the disease and getting people in treatment. These treatments can prevent liver disease, and reverse many of the early stages of it, if already beginning.
In our recent study, led by Heather Sperring, MS, a data quality specialist in the Center for Infectious Diseases and Public Health Programs at Boston Medical Center, between March and June 2020, we found that hospital-wide, testing of hepatitis C decreased by 50% and new diagnoses decreased by 60%. Primarily, the impact was in primary care clinics, where there was a 72% decrease in testing and a 63% decrease in new diagnoses. The emergency department and the inpatient units continued to see testing, but it was at a decreased volume, primarily because many patients were fearful about coming to the emergency department during the start of the pandemic.
The impact of such a significant decrease in testing and treatment affects both the individual patients as well as the larger population. A diagnosis allows for these patients to experience a timely transition into treatment, and it can guide patients to engage in safer practices, ultimately decreasing community spread of this easily-transmissible virus.
There is recognition among medical professionals that preventative care was delayed during the first COVID-19 surge, with possible severe consequences. What we saw during the first surge is not unique to hepatitis C, but reflective of what we saw for many different chronic diseases, including cancer diagnoses and the treatment of diabetes.
But things are different now than they were during the first surge. Providers, policymakers, and leaders in healthcare have learned about COVID-19, and we have taken that knowledge to work to make hospitals safe for both clinicians and the patients accessing preventative care. Providers must encourage all patients to continue getting the care that they need and reassure them that it can be done safely.
The good news is that it takes some time before we see the consequences of undiagnosed and untreated hepatitis C virus. This means that it’s not too late — even in patients who may have contracted the virus during the first surge, but haven’t yet been diagnosed. There is still time for us to diagnose, treat, and prevent liver disease from occurring.”


