A Free App Breaks Barriers to Prescribing Medication for Opioid Use Disorder
April 8, 2021
BMC's Office Based Addiction Treatment Program
With the removal of the X-waiver, more doctors and nurses can prescribe buprenorphine to patients with addiction. This tool from BMC can help.
Decades of research has demonstrated that life-saving medications for addiction, such as buprenorphine, greatly reduce the risk of all-cause mortality and overdose death in people with opioid use disorder (OUD). However, medications available to treat OUD and save lives, including buprenorphine and naltrexone, are consistently underutilized. A 2018 JAMA Pediatrics study showed that only 25% of commercially insured young adults with OUD between the ages of 13 and 22, and 5% of Medicaid-insured young adults with OUD of the same age, received life-saving medication for addiction. Results of another 2018 study published in Annals of Internal Medicine demonstrated that only 3 out of every 10 opioid overdose survivors received buprenorphine or naltrexone.
Now, as of this month, January 2023, the official removal of the X-waiver needed for clinicians to prescribe buprenorphine means that a major hurdle to helping people access this medication is gone. Expanded access to medication is imperative to reducing drug-related overdose deaths. But even with the X-waiver requirement removed, many physicians feel ill-equipped to prescribe the opioid use disorder medication.
A team at Boston Medical Center has been at the forefront of helping more providers get trained to prescribe buprenorphine. These efforts began in 2003, when the Federal Drug Administration approved buprenorphine to treat OUD. That year, under the leadership of Colleen LaBelle, MSN, RN-BC, BMC’s Office Based Addiction Treatment (OBAT) program was established, integrating addiction treatment into primary care. The nurse care manager model of treatment helped increase access to medication treatment for OUD and decrease the stigma around addiction, reinforcing the message that substance use disorder is a chronic condition that can be medically managed just like heart disease or diabetes.
As director of the program, LaBelle and her team oversee implementation of the OBAT model at federally qualified health centers in Massachusetts, creating the Grayken Center for Addiction Training & Technical Assistance (TTA) program. In 2020, the team provided training on evidence-based addiction treatment to ore than 14,000 individuals.
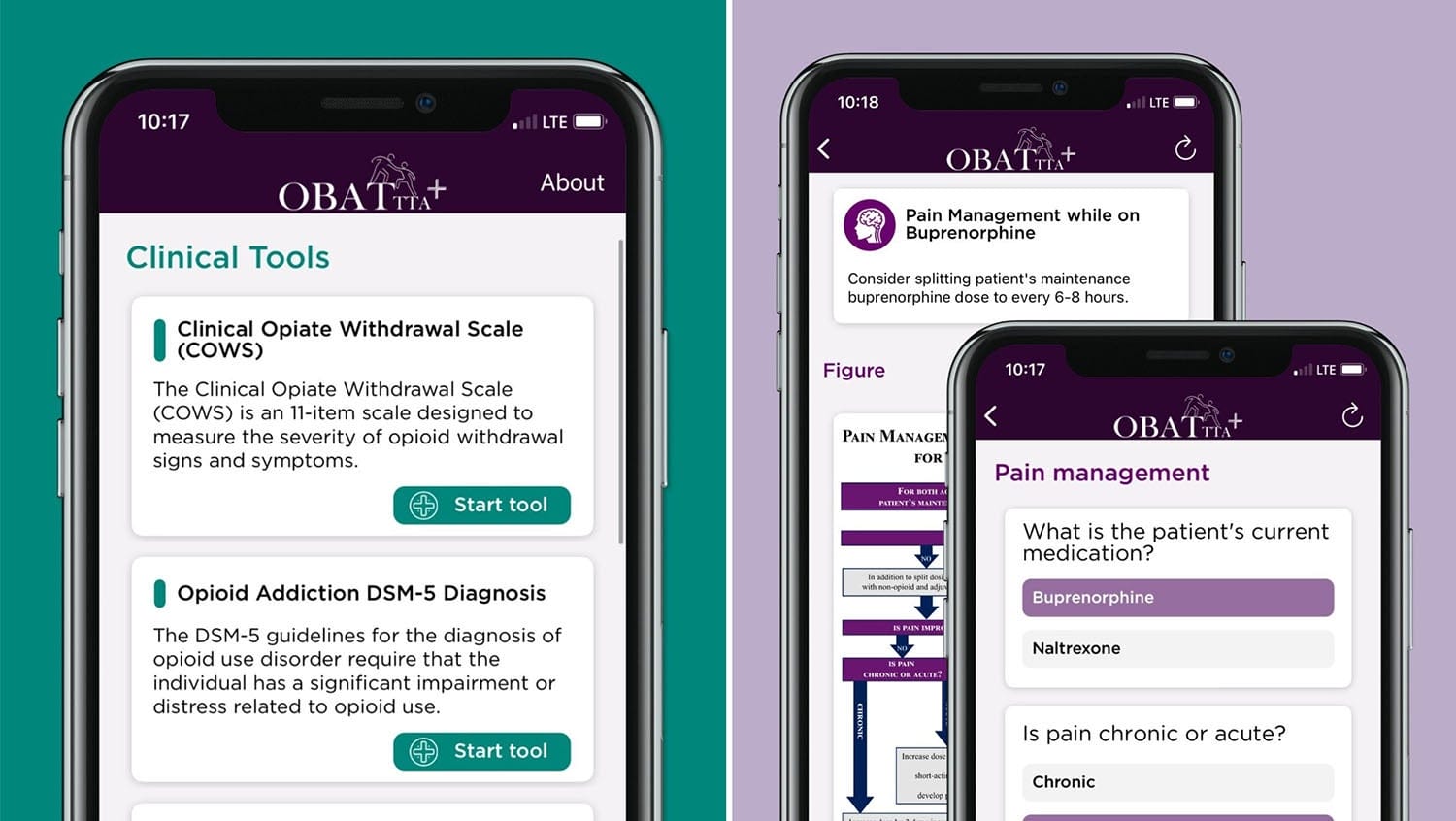
In 2021, LaBelle and colleagues at BMC, with funding from the Massachusetts Department of Public Health and the Opioid Response Network, developed an innovative mobile application, BMC MAT Quick Start, that brings their resources directly to providers. The app, which can be downloaded free of charge in the Apple App Store and Google Play, provides guidelines and resources about how to treat OUD with medication (buprenorphine or naltrexone) in office-based settings. HealthCity spoke with LaBelle after the launch of this app to get insight on this application and its role in helping expand access to treatment.
HealthCity: Data shows that the opioid crisis got worse amid the COVID-19 pandemic. According to the Center for Health Statistics, in the 12-month period ending July 2020, approximately 236 Americans died each day as a result of a drug-related overdose death — the highest on record. What needs to change in order to make progress here?
Colleen LaBelle, MSN, RN-BC: This is a critical time that requires us to pull out all the stops to provide treatment on demand, meeting people where and when they are at. Opioid use disorder is a life-threatening disease, and telling patients to come back later, giving them a referral, or telling them to call a given phone number doesn’t cut it. Treatment needs to be available at any door where a patient presents, but providers need the tools and the evidence-based guidelines to make that happen.
HC: Why did you develop the BMC MAT Quick Start app?
CL: We know from the data that less than 10% of primary care providers have a waiver to prescribe buprenorphine, and of those providers, only 6% are waivered to treat up to 275 patients, 22% can treat up to 100, and 72% can treat up to 30 patients. The low uptake in waivered providers is just one of the issues here. Only 13% reported prescribing close to their limit, according to a 2018 survey of DATA-waivered providers.
Many providers are reluctant to treat opioid use disorder, feeling ill-equipped to do so due to a lack knowledge and training in caring for patients with substance use disorder. They look to technology and easily accessible tools to help inform their clinical decision-making and address any concerns they may have regarding the treatment of OUD.
HC: How does the app work? What features and information can provider’s access?
CL: The app includes interactive clinical algorithms that helps walk providers through each step of the decision-making process when caring for patients with OUD. These interactive algorithms help healthcare providers make decisions on how best to approach treating their patients with OUD and manage chronic pain for someone with a history of substance use. The app also gives access to several tools, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM–5®) diagnostic criteria for OUD, the Clinical Opioid Withdrawal Scale (COWS), and the Alcohol Use Disorders Identification Test (AUDIT-C).
Q. What impact do you hope this app will have on clinical practice?
CL: We hope the app will increase access to evidence-based recommendations for treating OUD using medications. Additionally, we hope the app will help providers become more comfortable with the induction/initiation processes and pain management protocols for this patient population, treating OUD just like any other chronic life-threatening disease.
This article was originally published in April 2021. It’s been updated with news of the removal of the X-waiver.
For clinicians looking to prescribe medication for opioid use disorder and who need assistance, visit the Grayken Center for Addiction TAA’s MAT Quick Start tool.


