Rapid ACCESS Is Filling the Gaps for Patients With Addiction
October 11, 2022
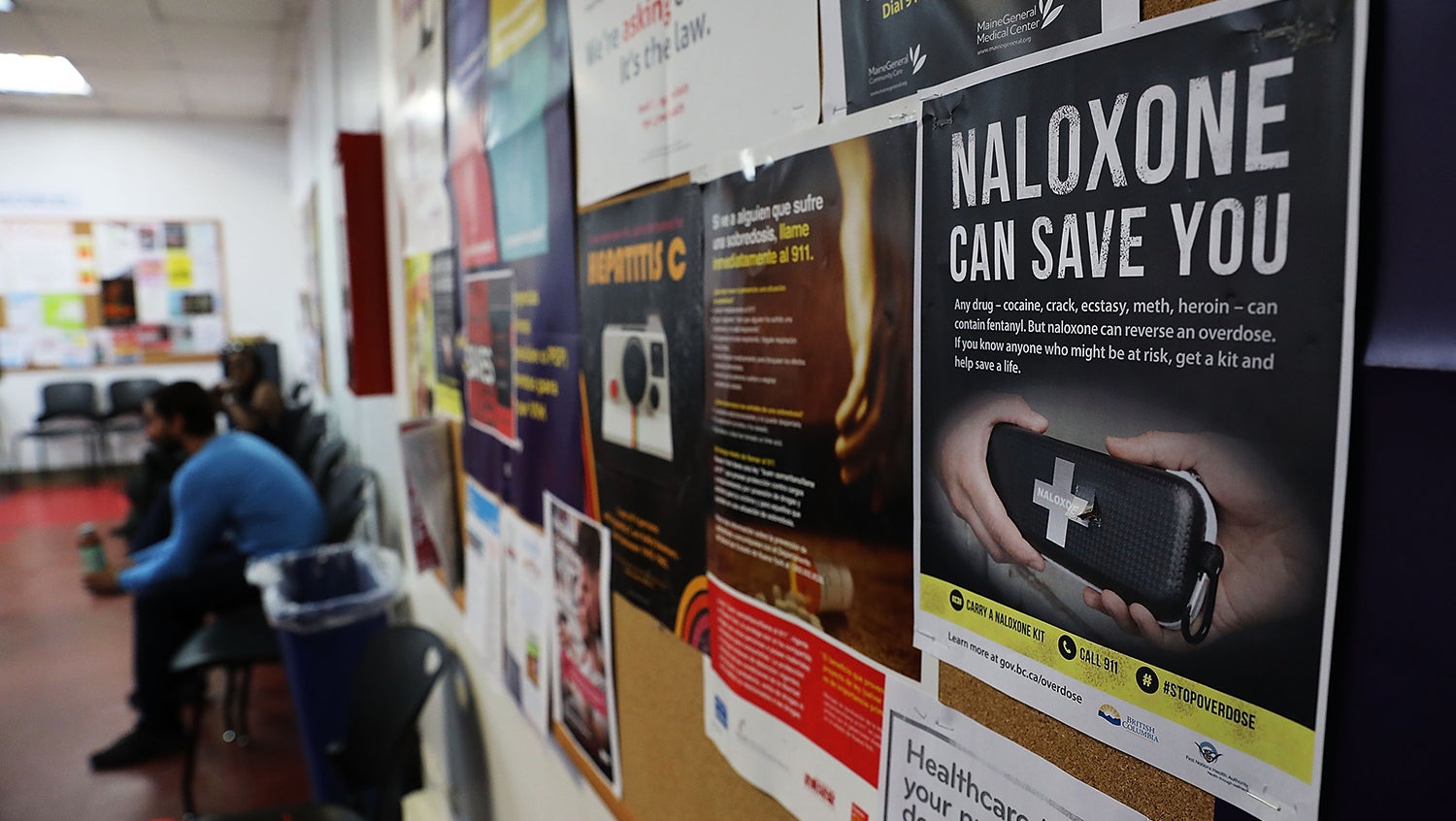
Spencer Platt, Getty Images
The program's recovery coaches meet substance use disorder patients where they are and help them navigate the array of services to suit their personal needs.
Those with close knowledge of recovery from drug or alcohol addiction know that effective treatment cannot take a one-size-fits-all approach — it has to meet patients where they are, no matter their stage of readiness.
Research suggests that 40 to 60% of people on the recovery path will experience relapse. The stigma associated with addiction can keep people who need help in the shadows. Add to that a fragmented addiction care industry, a dearth of tools to help patients navigate a maze of treatment options — and even unscrupulous actors who prey on people with substance use disorders (SUDs) — and it’s no wonder that long-term recovery can feel so elusive.
The Grayken Center for Addiction at Boston Medical Center provides a robust range of addiction treatment programs on-campus and off, but even so, patients with unstable life circumstances aren’t always able to fully access all the help that’s available. Some arrive at the Emergency Department (ED) for substance-related health crises, but then disappear from the system without engaging in substance use disorder treatment. Others engage with one service but have difficulty following up on referrals or navigating from one program to the next — essentially, falling through the cracks.
In 2021, the Grayken Center launched Rapid ACCESS (Assessment, Connection, Counseling, and Engagement with SUD Services), to fill as many of those cracks as possible. The program’s hotline team receives referrals and reaches out to patients to assist them in connecting to services. Then, trained recovery coaches step in to provide the compassionate support and assistance patients need.
“Patients were coming here to BMC and being offered these services, but there was no ‘in-between’ to walk the patients through the process,” says program manager Sandra Honter Williams, MBM. “Rapid ACCESS was designed to be a bridge program where BMC providers could refer patients, so that we could help them navigate what treatment pathway best works for them.”
Patients come to Rapid ACCESS through various BMC programs, including Project ASSERT, which screens and counsels patients in the ED, the Addiction Consult Service, which works with inpatients and helps transition them to post-hospital treatment, Faster Paths to Treatment, an SUD urgent care program, and Project RESPECT, which serves pregnant and postpartum patients. Once in the Rapid ACCESS program, patients work with a recovery coach for up to 90 days.
Using a harm reduction model of addiction treatment
Williams emphasizes that Rapid ACCESS uses a harm reduction model, with no pre-set expectations that patients will stop using drugs or be ready for recovery. “We meet them where they are,” she says. “The patient is the one who tailors this program.”
Rapid ACCESS recovery coach Robyn Phillips sees patients in a wide range of readiness stages and adapts her guidance for each person.
“If they’re willing to enter recovery, I’ll ask, ‘What would you like this to look like?'” she says. “And whether they want MAT [medication for addiction treatment], programs like AA or Narcotics Anonymous, Smart Recovery, a religious method — whatever pathway they want to go down, I’m here to support them.”
Some patients are far enough along to be seeking a job, and she helps them with résumé preparation or mock interviews. Others are not even at what she calls the starting line. “If they’re not at the point yet to enter recovery, if they still want to use, then it’s, ‘Okay, how can I help you use more safely than you are now?”” she says.
Certified recovery coaches build trust, structure for those in recovery
Like all the program’s recovery coaches, Phillips completed training to become a Certified Addiction Recovery Coach. She also holds a certificate for substance use disorder counseling that she earned in 2013 and has prior experience as a case manager in other programs.
Once linked with a patient, she keeps in close touch. “If they have a phone, I’ll always call and check in. If I don’t hear from them, I’ll call and say, ‘Hey, how are you? I haven’t heard from you. What’s going on?'”
But all of that comes after initial trust-building.
“A lot of times, patients have had bad experiences with reaching out for help. They’ve had a lot of trauma. They don’t even trust themselves at the moment,” Phillips says. “So it takes some time to build that trust up, so they know that I’m going to be there and I’m going to support them any way that I can.”
Phillips can relate. She’s in recovery herself, for six and a half years now, though she first started addiction treatment 10 years ago. She knows the feeling of finishing a program and having no idea what comes next.
“Once you leave the residential program, all that support that you had in there is gone,” Phillips says. “You need structure, and you need to have a network and stay connected, especially at the beginning. It’s very important.” Now, she can offer others the helping hand she knows they need.
She mentions one patient she met last winter, a woman who was living in a tent encampment not far from BMC. “She was really, really down. She wasn’t in recovery yet. She was still actively using. But she kept showing up. And the fact that she kept showing up meant something in her wanted to change,” she says.
“Every time she’d come, I’d just give her a cup of coffee and we’d sit there and chat,” she recalls. “Then, as those days went on, she wanted to enter detox.”
So Phillips connected her to detox services. It took more than one try, but eventually it worked. Today the woman is in a program that helps her get housing and has even returned to her trade as a sous chef.
“She wasn’t working. She didn’t have a home. She didn’t have anything when she first came through the door,” Phillips says. “And now she’s in a program that’s helping her.”
Rapid ACCESS’ impact so far and what’s next
As of the first 14 months of Rapid ACCESS, recovery coaches had served 383 patients, with the average duration in the program 58 days, according to Grayken Center Project Manager Allison Blakemore.
Blakemore’s team is tracking several metrics: number of ED admissions pre- and post-engagement with Rapid ACCESS; severity of ED admissions; program connections; treatment engagement with other programs; and connection to long-term outpatient treatment. Outcome data is still being processed, but what the team has seen so far is promising.
“We work with very high-risk patients that are often more challenging to engage or connect to other treatment programs,” Blakemore notes. “[But] we have been able to connect over 100 patients to long-term outpatient treatment after discharge from our program.”
While the program is having a positive impact already, Williams has plenty of ideas for what could be added.
High on her list is to expand staffing. Currently, among the recovery coaches, one has Spanish language fluency and one specializes in youth. Williams wants to expand on specialties offered — for instance, additional languages to fill even more cracks that can make patients fall out of treatment.
She also envisions greater capability to connect patients to housing and extending the program’s reach by working within drug courts and other programs.
“My dream would be to see Rapid ACCESS at the table in drug courts, at CSSs [clinical stabilization services], at the long-term treatment programs, and where people are coming out of incarceration,” she says. “Why? Because when it’s time for you to come out, that’s a major adjustment. A recovery coach could be there to support you as you’re transitioning back into society — somebody that has lived experience, knows what you’re going through, will meet you where you’re at, and will not judge you if you relapse.”
To refer a patient or talk to experts about the addiction services at Boston Medical Center, including Rapid ACCESS, call our connection hotline at 617-638-5500.
This story has been updated from its original version, published in October 2022, to include more information for referring providers.


