Getty Images
Esophageal cancer outcomes differ at safety net hospitals compared to hospitals without a high safety net burden, but why?
SO WHAT? | Findings suggest that poorer esophageal cancer outcomes at safety-net hospitals are not likely due to the care available at the institutions but rather to factors that present greater barriers to care for the vulnerable patient populations at these hospitals, such as comorbidities, housing status, and supportive care. To mitigate the impact of these factors, safety-net hospitals should consider creating targeted clinical pathways for improving delivery and access to esophageal cancer care.
CONTEXT | Certain factors, such as being Black, Hispanic, or low-income, have been associated with decreased use of curative therapy and higher rates of death for people with esophageal cancer. These low-income and minority patients are treated more often at hospitals with a high safety-net burden.
STUDY OBJECTIVE | Determine the impact of a hospital’s safety-net burden on the disparities in presentation, treatment, and outcomes of patients with esophageal cancer.
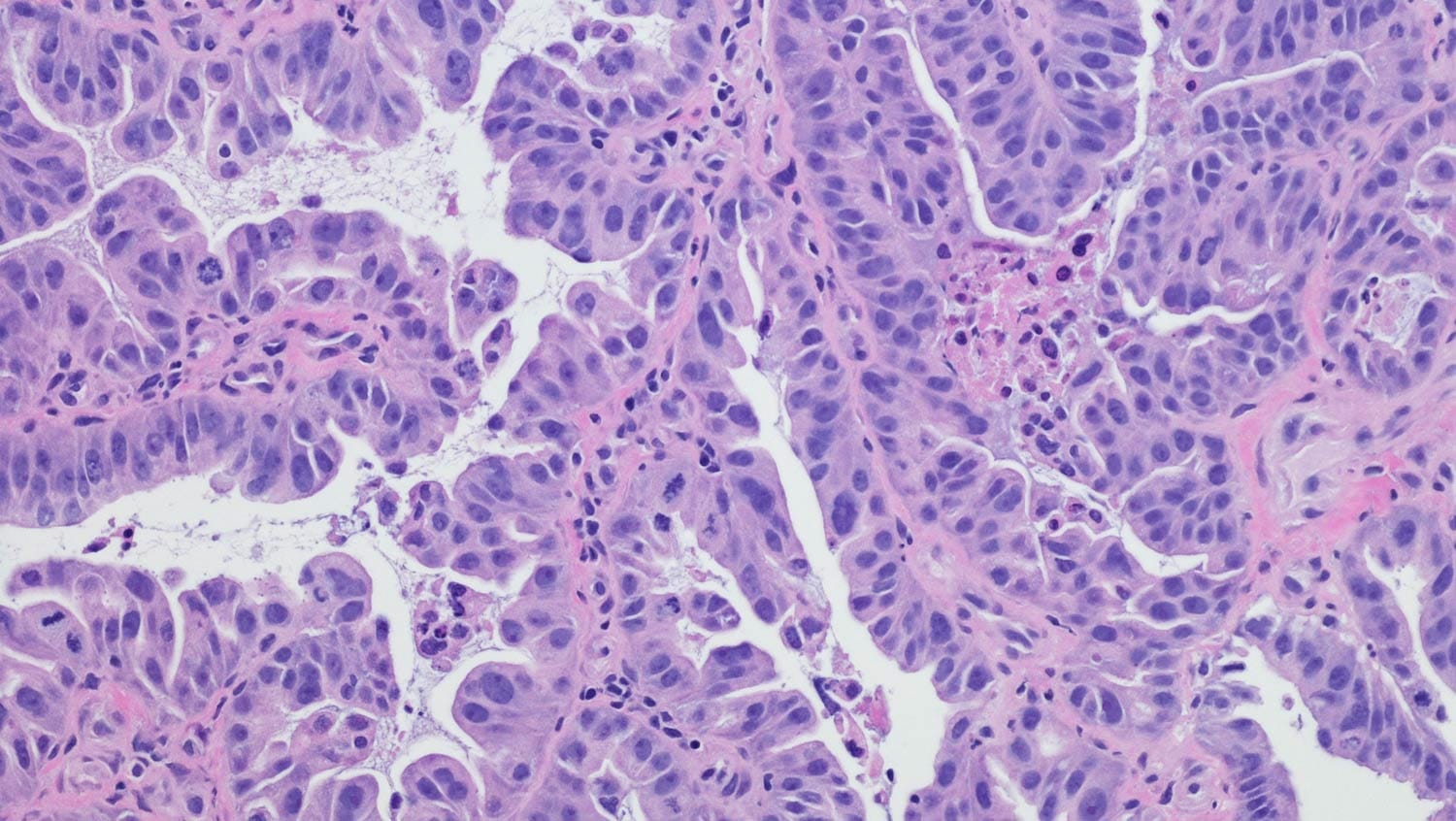
FINDINGS | Hospitals with a high safety-net burden saw a greater proportion of patients who sought treatment at later stages of disease. These hospitals were associated with an 11% higher risk of death than low-burden hospitals, but only for patients with squamous cell esophageal cancer. For adenocarcinoma, which accounts for more than 80% of esophageal cancers, the researchers found no difference in survival rates among hospitals with a low, medium, or high safety-net burden. Mortality risk was not associated with race or ethnicity.
DATA SOURCE | National Cancer Database data (2004-2013) of 56,115 patients with esophageal cancer treated in 1,215 hospitals.
PULL QUOTE | “While our findings may suggest that the mortality risk associated with high-burden hospitals may be attributable to these facilities, the limitations of this analysis should temper this interpretation. We excluded nearly 17,000 patients with missing covariate data. The inclusion of this cohort could significantly attenuate, and perhaps nullify, the association of mortality with high-burden hospitals.”
Authors: Sridhar P, et al.
Source: Esophageal cancer presentation, treatment, and outcomes vary with hospital safety-net burden. (2018). Annals of Thoracic Surgery.


