‘The Sky is the Limit’ for Who Could Benefit from BMC Brighton’s New Surgical Robot
August 18, 2025

Jeff Fernandes, Boston Medical Center
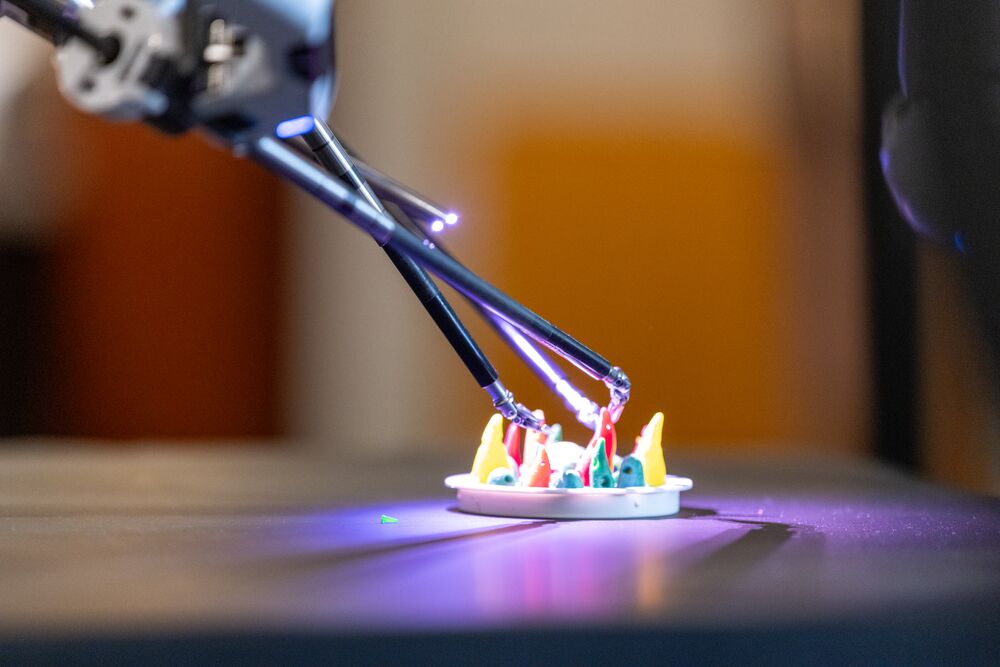
The da Vinci 5 surgical robot in demonstration by Dr. Stanley Tam, Chief, of Cardiothoracic Surgery at Boston Medical Center – Brighton.
Michael O’Connor became a thoracic surgeon because he knew he wanted to join a dynamic and evolving field where he could treat people living with cancer. Advocating for his patients and his colleagues, he pushed for BMC Brighton to evolve as well, and helped the hospital upgrade its robotic surgery system to the “latest and greatest.”
Like many clinicians, Michael O’Connor, MD, got into the field because he wanted to make a difference. He started medical school a little uncertain, and completing his rotations, he was still unsure where he’d find a fit for his career. It wasn’t until the last rotation of his third year, when he worked in a surgical oncology service, that he knew he had found his home.
“I really loved taking care of cancer patients because they’re often people who may have otherwise been healthy, taking care of themselves, and they get a diagnosis that just changes their lives,” O’Connor says. “They’re invested in their care and their care team’s advice, and with the responsibility and respect these patients have—I wanted to take care of them.”
Unlike the kickoff to medical school, O’Connor then entered his residency clear-eyed and set on surgical oncology. It was a lot quicker this time—year one—that he again found his niche. Thoracic surgery, providing diagnosis and treatment for a range of cancers and other conditions affecting the lungs, esophagus, and chest.
Finding his passion in a growing field
Thoracic surgery is a growing and evolving field. Just 10 or 20 years ago, O’Connor explains, lung cancer was mostly diagnosed at Stage IV—meaning it was already inoperable. Due to advances in screening protocols, there is a new group of people living with lung cancer who can be treated with surgery.
“Our knowledge of treating this disease has grown exponentially in the last 15 years,” O’Connor says. “I saw it as a field that I could be taking care of cancer patients, who I enjoyed taking care of, but also make a big difference.”
Because of this exponential growth over a short period of time in the number of treatable patients living with lung cancer, there was a shortage of physicians who were capable. Dr. O’Connor knew he wanted to add himself to that roster of physicians who could help people living with cancer not only be treated but recover and add years to their lives.
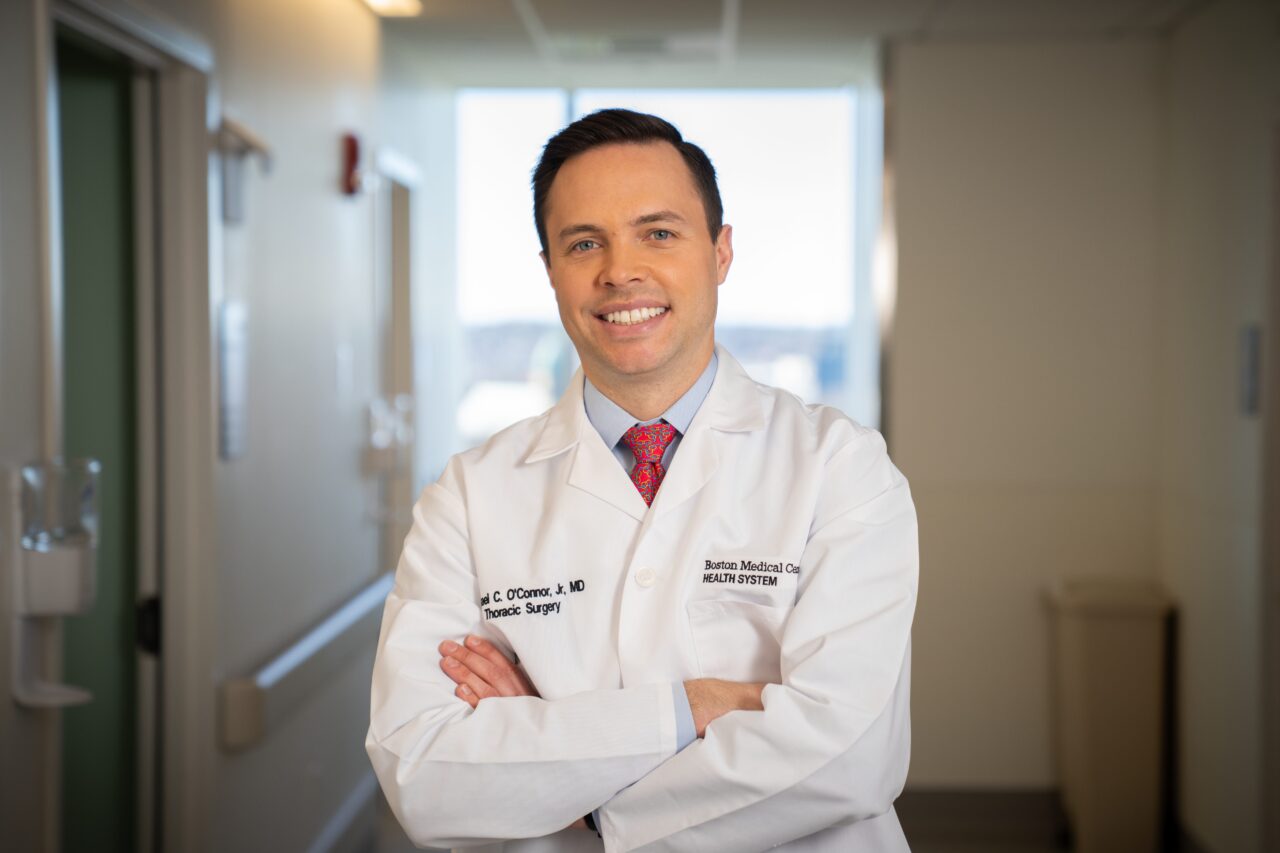
Training and working in Chicago, Dr. O’Connor focused on minimally invasive and robotic procedures to not only treat cancers like lung and esophageal, but also all sorts of other chest problems, like pericardial and mediastinal diseases—the sac surrounding your heart and the chest cavity between your lungs, respectively.
“It was a field that I saw continuing to grow, continuing to innovate. I felt like I could make an impact,” he says.
Maybe somewhere in the back of his mind, he was inspired by his grandfather’s best friend—a cardiothoracic surgeon who O’Connor had become quite close to, particularly after his grandfather passed away. When he was young, O’Connor would visit his grandfather at his office, which he shared with his best friend. His grandfather was a primary care physician, the only person in healthcare in his family, and a major influence in his life.
“I’m not sure if he’d be turning over in the grave knowing I’m a surgeon,” he jokes.
The da Vinci 5 comes to BMC Brighton
When he joined the team at Boston Medical Center – Brighton last fall, he wanted to bring this expertise in minimally invasive robotic surgeries from the massive academic hospitals in big cities to the community, where people could access cutting-edge care close to home.
“It’s easier for their family to come and be with them during a difficult time,” he says. “Most of my patients really only spend around one or two nights in the hospital, but still, all chest surgery is fairly major surgery, and having family around for support makes a big difference.”
O’Connor arrived at his new home when it was hitting a major turning point. At the time known as St. Elizabeth’s Medical Center, the hospital had just joined BMC Health System after a period of tumult that included a lack of resourcing. The hospital had an older model of a robotic-assisted surgery device, and O’Connor focused on advocating for an upgrade to benefit not only the surgeons, but also the patients and the hospital’s bottom line.

“The administrations at BMC as well as here at BMC Brighton were not only interested in investing in a new machine, but they also wanted to get the latest and greatest,” he says.
O’Connor went to test out the da Vinci 5 (DV5), Intuitive Surgical’s latest and most advanced robotic surgical system. What he was most impressed by was the “force feedback” technology—meaning that it uses haptics to mimic the vibrations, pressures, and other forces a surgeon senses when operating inside the body, simulating the sensation of touch and texture. It helps match the surgeon’s visual cues to their tactile experience, making a more realistic experience for surgeons.
Thanks to O’Connor and the team’s support, the DV5 came to BMC Brighton this month, making it one of only five hospitals that use the technology in all of New England. The first local patient was treated with the robotic surgery on Thursday, August 14, by O’Connor’s colleague Dr. Eduardo Vega, and the team has completed multiple additional surgeries with the da Vinci 5.
Robotic surgery brings advantages to patients and hospitals
As O’Connor advocated, the DV5 technology can be of great benefit to patients and the hospital, not just to the surgeons.
The force feedback aids in applying significantly less force to tissue than without force feedback. This means surgeons are less likely to cause compression or injury to tissue—for example, the lungs—causing less damage and inflammation, less need for oxygen, and ultimately a shorter recovery.
For patients and their families, they’ll experience shorter times in the operating room and shorter overall recovery time. Not only does that mean less time under anesthesia, which lessens their risks; it means getting back up and, on their feet, more quickly.
“The technology has made patient’s care much less of a burden on them, in terms of recovery,” O’Connor explains. “Patients used to spend a couple weeks in the hospital. Now, they spend an average of one to two days, and most people are going home the next day. And the minimally invasive approach, without big incisions, makes a big difference for people.”
Shorter OR times, shorter hospital stays—all of this also impacts the hospital’s bottom line, which means they can reinvest money back into patient care.
Who exactly can benefit from DV5 robotic surgery?
The DV5 was first invented for cardiac surgery, but its use has expanded to many different fields. Gynecologists, urologists, bariatric surgeons, and thoracic surgeons like Dr. O’Connor are now using this cutting-edge technology to benefit their patients. It’s being used to treat everything from hernias and gallbladders to complicated oncology cases, including liver and pancreatic surgery. In other parts of the world, surgeons are using it for minimally invasive mastectomies for breast cancer patients, and others using it for neck and thyroid surgery.
“I’m sure our use of the DV5 will continue to grow and expand as BMC and BMC Brighton partner to take care of our communities,” O’Connor says. “The future direction for our field, for general surgery, has been expanding. People are using robotic surgery, and the DV5 in particular, for more things, and the sky is the limit in terms of who could benefit from it.”
This story included contributions from Isabella Bachman, Manager of Content Strategy at Boston Medical Center Health System.


