Transcranial Magnetic Stimulation Therapy Offers New Hope for People with Depression
December 11, 2025
By Meryl Bailey

Isabella Bachman, Boston Medical Center
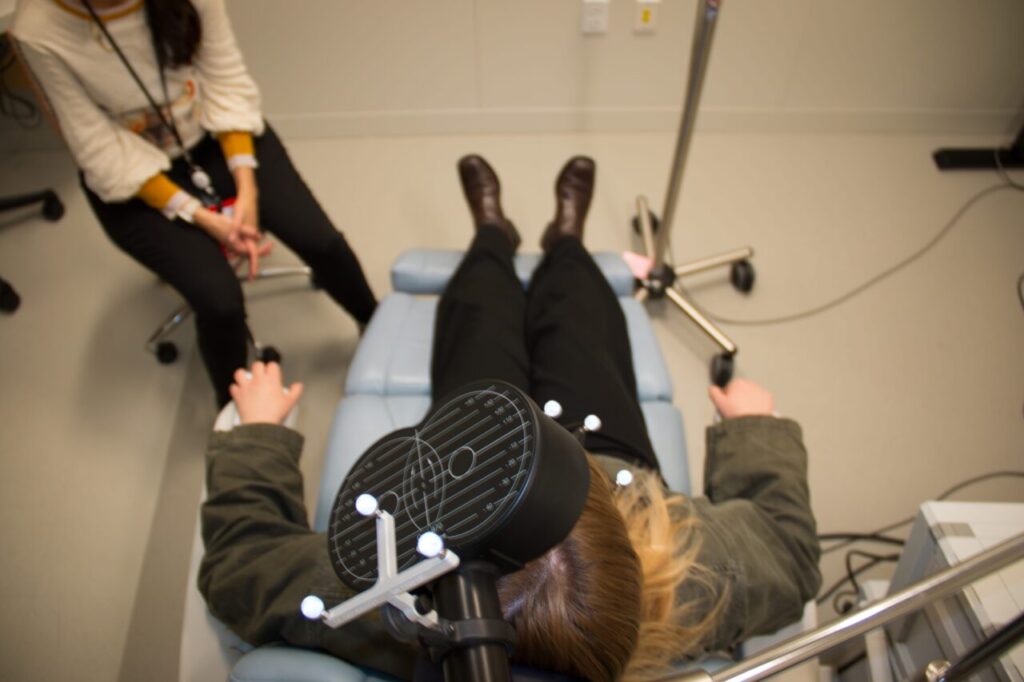
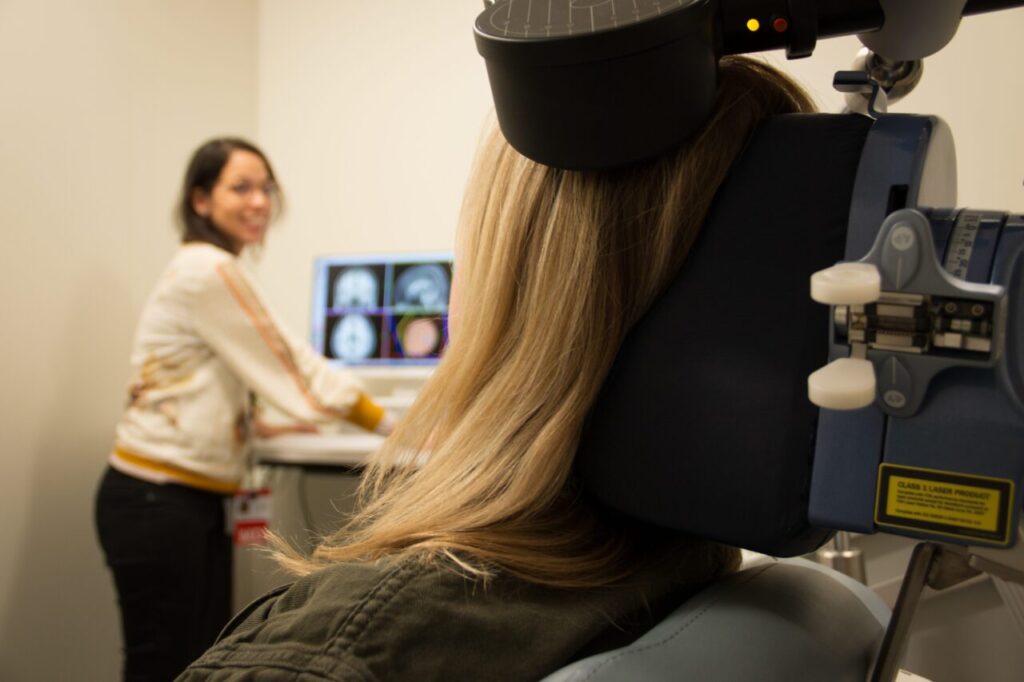
Anna Maria Rivas-Grajales, MD, director of BMC's Transcranial Magnet Stimulation (TMS) Clinic, and clinic worker simulate a clinic appointment.
When other treatments fail, TMS therapy is a promising, evidence-based alternative for patients with major depressive disorders.
Ruth Rodriguez’s depression hit in her late 20s. Under her doctor’s supervision, she tried medication after medication over the years, yet her condition remained unshakeable. At 35 and a single mother of two young children, she was overwhelmed managing work, family, and her mental health.
“I was very depressed, very sad,” Rodriguez remembers, in a call with HealthCity.“ And if I had any synchronous problems with family or work, I’d have a hard time going through it; I’d see things bigger than they were.
Rodriguez’s experience is far from unique. An estimated 31.4 million Americans aged 18 to 65 reported a major depressive disorder in 2023. Among those, about 30% are resistant to treatment, including medications and different therapy modalities. Treatment-resistant depression (TRD) is linked to lower quality of life, unemployment, higher chances of relapse, and disproportionately high healthcare costs, which poses severe economic burdens for patients.
For patients with depression that’s resistant to treatment, like Rodriquez, transcranial magnetic stimulation (TMS) offers a hopeful alternative. FDA-approved for treatment of depression since 2008, the non-invasive procedure harnesses electromagnetism to stimulate nerve cells in the brain that regulate mood. For people that undergo the treatment series, studies show remission rates of up to 40%.
Increasing access to transcranial magnetic stimulation
Traditionally limited to private practice settings, Boston Medical Center (BMC) is one of the few essential hospitals nationwide to offer TMS. By integrating the therapy into this type of setting, BMC is working to bridge the gap between medical innovation and the populations who bear the heaviest burden of depression. This has been a critical gap, as mental health research consistently finds an association of higher prevalence of depression with low socio-economic status. A U.S. Centers for Disease Control and Prevention survey found that people living below the poverty level are 2.5 times more likely to suffer from depression than people with more resources.

Ana Maria Rivas-Grajales, MD, director of BMC’s Transcranial Magnetic Stimulation (TMS) Clinic, has seen promising results so far. Her clinic teams are seeing response rates of 45% to 50%—which is far higher than the chances of patients responding to a fourth, fifth, or sixth medication trial, after not responding to others, which is around 5% to 10%.
“TMS could be much more effective than putting a patient through another medication trial,” Rivas-Grajales says.
Barriers to TMS therapy treatment for patients
TMS’s recent inclusion in insurance plans, including Medicare and MassHealth, is helping expanding access to many more people who could benefit from it. Still, barriers remain. Rivas-Grajales explains that the procedure is a time commitment.
At BMC, patients can expect to undergo daily treatment for six to eight weeks. The treatment itself lasts about 10 minutes, and patients can expect a total visit to range from 20 to 30 minutes.
With this level of commitment, patients are investing time and travel into their care. It may require a certain level of stability or wraparound support during those six to eight weeks to complete. Which is why it’s so crucial for essential hospitals and other health centers experienced in providing additional support structures to continue to invest in this potentially transformational therapy. But not all barriers are real, says Rivas-Grajales.
“I think access is also an issue about perception.” says Rivas-Grajales about increasing provider awareness, “Some providers might not refer patients to TMS thinking, well, patients probably have to be out of pocket. Or maybe that a treatment location might be too far away from where they live.”
In addition to the provider’s perception, funding also has arisen as a perceived obstacle—one that Rivas-Grajales hopes systems will reconsider.
“There seems to be an implicit bias toward mental health conditions when it comes to funding from institutions and from insurance companies. It is surprising because multiple hospitalizations of a patient with chronic depressive symptoms throughout the year are higher than what an entire course of TMS would cost,” she says. “Being more open to this type of intervention would be greatly beneficial financially in the long term.”
Rodriguez’s experience models benefits of TMS therapy
Rodriguez became curious about TMS after witnessing the transformation of a close friend with depression who underwent the treatment. Her psychiatrist referred her to BMC’s TMS Clinic, where she met with the team to discuss her candidacy and undergo an evaluation. Her brain was measured and mapped for the optimal placement of the electromagnetic coil. Over the next two months, she visited the clinic every weekday for 10-minute TMS sessions. Beyond some sensitivity to her scalp, she says the outpatient procedure was painless. Rodriguez noticed an improvement in her symptoms after two weeks.

Rodriguez’s treatment experience is typical, notes Rivas-Grajales. Patients can begin to see results as early as two to three weeks of starting treatment, although response trajectories vary among individuals and maximal benefit generally requires a full course of treatment. Most patients experience symptom relief months after completing treatment, and nearly half remain in remission at one year.
Six months from the start of her treatment, Rodriguez considers TMS life-changing. While she kept taking medication for depression during the therapy, she is working with her psychiatrist to slowly reduce and eventually stop. She feels more present with her children and in her role as a clinical researcher in internal medicine. Her focus and motivation are restored. She is currently studying to take the medical board exams.
Dr. Rivas-Grajales is hopeful that TMS will grow to become a standard secondary prevention therapy for depression, not only work reducing the burden of major depressive disorders on health systems, but also most importantly helping more people return to life.
“I started to notice how I was reacting differently to situations,” Rodriguez says about how she felt just a few weeks after completing the TMS treatment at BMC’s clinic. “I started to understand that other people’s problems are not mine and could just let go of things and not take them personally. I was able to pay more attention to work and studying and be more productive because I wasn’t taking on that heavy of an emotional burden anymore.”


