Getty Images
With systemic shortcomings in addiction medicine training on full display, experts find new ways to share knowledge with those providing care.
COVID-19 has painfully exposed the vulnerabilities of the American healthcare system, but it’s also revealed areas ripe for innovation and ways to care for patients more efficiently and effectively. One area that has both revealed unpreparedness and inspired innovation is substance use disorder (SUD) treatment.
The number of patients with substance use disorder who are now necessarily engaging with the system because they have COVID-19 has underscored the significant gap in addiction medicine training among providers tasked with caring for these patients, addiction medicine experts say. While nurses and physicians have stepped up to help in the pandemic, many have discovered they were not formally prepared with the skills needed to address patients’ comorbid SUDs. In fact, an estimated 8% of the population over age 12 has a diagnosable substance use disorder, yet a majority of providers feel they’re unprepared to treat SUDs.
A recent survey found that only 1 in 4 healthcare providers in Massachusetts received addiction training as part of their medical education. Among surveyed internal medicine and emergency medicine providers, less than half believed that opioid use disorder is treatable at all. The lack of training combined with the stigma attached to addiction is a troublesome combination as providers seek to steer patients away from costly for-profit programs, which have shown to be little to no help, and toward evidence-based medical care.
“It doesn’t matter what field of nursing or what field of medicine you want to go in, what your specialty is going to be, or where you’re going to practice — you’re going to have patients who have substance use disorders, and you need to know how to approach it,” says Kristin Wason, a nurse practitioner and clinical educator for the Office Based Addiction Treatment (OBAT) Program at Boston Medical Center.
A case example
The training issue hit hard when the COVID-19 outbreak began to take hold. As nurses, doctors, and providers from a variety of disciplines began working outside their fields of expertise to help with the crisis, many were faced with learning on the job how to treat patients with substance use disorders. Nowhere was the issue more pressing than when Boston Medical Center reopened the neighboring East Newton Pavilion building, which had been closed and sold to the state, as a COVID-19 recovery center for the homeless community. Many nurses and providers had to get up to speed quickly on how to recognize addiction symptoms, proper techniques for dealing with withdrawal, and the latest harm-reduction methods.
Related read: For Hospitals, a Blueprint for Fighting the Opioid Epidemic »
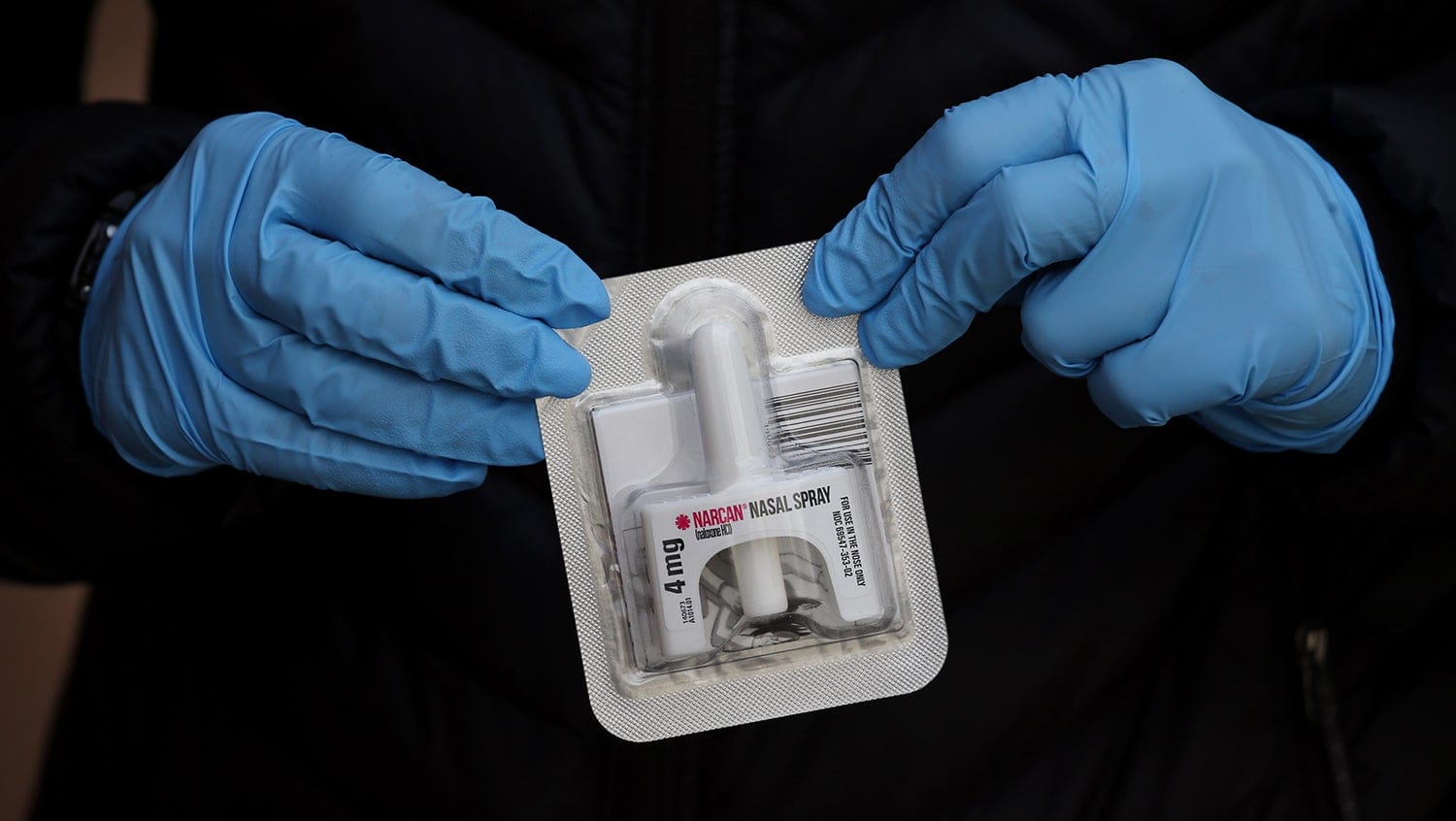
It became clear that some nurses had no experience delivering opioid use medications such as buprenorphine or methadone. Others were unfamiliar with the dangers of alcohol withdrawal. Some had questions about when and how to distribute clean needles or Narcan, or whether they were even allowed to.
This lack of knowledge is not a shortcoming at the individual level, however. Systemically, this type of training is still not a priority, even as the opioid crisis has grown ever more pressing.
“There’s no mandate, no requirement to teach about addiction,” Wason says. “And that’s really unfortunate. Everything I learned about addiction medicine, I learned doing the work and by talking to patients. Nurses are teaching each other, and the patients are teaching us.”
To fill immediate training needs, Wason and her OBAT team have organized regular Zoom calls and weekly online check-in meetings featuring leading addiction experts to go over protocols with frontline providers. The meetings are joined by people in diverse roles, including recovery coaches, social workers, nurses, advanced practice providers, and physicians, and include a 10- to 15-minute didactic followed by an open dialogue for providers with specific case questions or who need guidance.
Related read: ‘Meth Is Here and Now’: A Growing Presence in the Opioid Crisis »
The calls have become a valuable resource, and perhaps even a safe haven, for providers without SUD training to ask questions openly, share experiences, and glean proper treatment methods and techniques from experienced providers. Topics have included how to handle overdoses, how to discuss treatment options with patients, what the different medication options are, and best practices in working with the homeless community, among others.
“What I find is that a lot of new providers and new nurses are hesitant or fearful about treating addiction,” Wason says. “They think it’s going to be so much work, and that the patients are going to be challenging forever.” Many healthcare providers have only seen the people who are really struggling, and not the ones in recovery, she notes. “But once they start doing it and they help people get into recovery, they realize how rewarding this work is.”
The reduced reliance on blood and urine toxicology screenings to identify drug and alcohol issues during treatment also highlights the need for more patient-centric addiction training. With fewer SUD patients being seen in person and more being monitored via telemedicine, nurses and doctors have had to rely on other methods to detect treatment and recovery issues. Wason hopes these methods can be incorporated into teaching models going forward.
“People are always very hyper-focused on the tox screens, but there are lots of other markers that show how well your patient is doing,” Wason says, reiterating that the goal of treatment is improving functioning and quality of life. “Are they presenting to their visits, whether that be in the office or remotely? How are they sounding when you’re meeting them? Are they engaging in other recovery services? Does it seem like their life is getting better?”
What’s next
There is some encouraging news that training is increasing: doctors with less than 10 years’ experience are twice as likely to have had addiction treatment training than those who have been in practice for 10-plus years. And the OBAT Zoom calls join several other initiatives to improve providers’ familiarity and comfort with addiction medicine, including their OBAT Training and Technical Assistance program and real-time guidance that’s available through the Massachusetts Consultation Service for Treatment of Addiction and Pain (MCSTAP) hotline.
But these initiatives, as helpful as they are, are only a start — there needs to be a comprehensive, long-term focus on addiction treatment training, Wason says.
“Everybody should be able to treat addiction medicine,” Wason says. “No matter where patients are entering the medical system, there should be people there that can help them. That is not what’s happening right now.”


